This article includes a list of general references, but it lacks sufficient corresponding inline citations. (September 2012) |
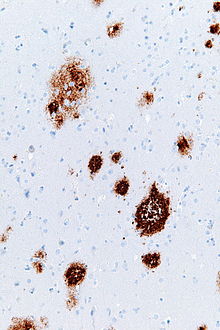
Senile plaques (syn. neuritic plaques, senile druse, braindruse) are extracellular deposits of beta amyloid in the gray matter of the brain.[1] Degenerative neural structures and an abundance of microglia and astrocytes can be associated with senile plaque deposits. These deposits can also be a byproduct of senescence, or biological aging, however large numbers of senile plaques and neurofibrillary tangles are characteristic features of Alzheimer's disease. Abnormal neurites in senile plaques are composed primarily of paired helical filaments, a component of neurofibrillary tangles.[2] The plaques are variable in shape and size, but are on the average 50 µm in size.[3] In Alzheimer's disease they are primarily composed of beta amyloid peptides. These polypeptides tend to aggregate and are believed to be neurotoxic.
Identification
editSenile plaques are visible in light microscopy after staining by silver, Congo red, Thioflavin, cresyl violet, PAS-reaction, and by fluorescence and immunofluorescence microscopy.[2][4] Bielschowsky silver stain was found to be the least efficient means to visualize senile plaques whereas Campbell silver and Gallyas silver showed approved identification accuracy. Using Congo red only one-fourth of senile plaques present were stained noticeably.[5] Senile plaques may also be visualized with an immunostain directed against beta amyloid. The primary problem with the above staining methods however is that sections of the neural tissue must be excised from the brain in order to accurately identify senile plaques. This is problematic because removing neural tissue can be as detrimental as the actual plaques themselves.
Formation and Description
editConcentrated in the synapse of neurons is an Amyloid Precursor Protein (APP) which is a type I integral transmembrane protein. A portion of this protein contains an Aβ peptide sequence. This region comprises part of exon's 16 and 17 of the 18 exon's spanning the gene contained on the Amyloid Precursor Protein.[6] There are three proteases that can process APP. However, only β- and γ-secretase have been directly implicated in the formation of senile plaques. β-secretase (BACE) analogous to a peptidase enzyme that catabolizes proteins and peptides. This secretase cleaves APP causing the formation of an ammonia, NH2 terminus. A soluble version of APP known as β-APP and a CT99 carboxyl terminal fragment is also produced. After much of APP has been released, γ-secretase proteolysis the remaining carboxyl fragments in the center of the transmembrane domain. The sequential actions of γ-secretase following BACE activity ultimately leads to the formation Aβ.[6] The pathway leading to the formation of an Aβ fragment is not an unnatural or abnormal occurrence. However, this physiological peptide can collect in the extracellular space. The accumulation of Aβ outside of neuronal synapses that aggregate form a mass known as senile plaques.
Occurrence
editSenile plaques can be found in human and animal brains (e.g. mammals and birds). From an age of 60 years (10%) to an age of 80 years (60%) the proportion of people with plaques increases approximately linearly. A small number of plaques can be due to the physiological process of aging. Women are slightly more likely to have plaques than men.[3] The plaques occur commonly in the amygdaloid nucleus and the sulci of the cortex of brain.
History
editBlocq and Marinesco first described plaques in the grey matter in 1892. Because of their similarity to the actinomyces druses they were called druse necrosis by Oskar Fischer in the beginning of the 20th century. The connection of plaques and demential illness was discovered by Alois Alzheimer in 1906. Bielschowsky supposed in 1911 the amyloid-nature of the plaques. Wisniewski denominated them neuritic plaques in 1973. The second half of the 20th century saw proposed theories of immunological and genetic factors in plaque formation.[7] Other factors in Alzheimer's disease verification include pathological neurofibrillaries, tangles, and atrophic brain with hydrocephalus. The formation and the distribution of the pathological neurofibrillaries have a regularity[8] Statistical investigations were performed by J.A.N. Corsellis and M. Franke in the 1970s. M. Franke showed that a demential disease is likely when the number of senile plaques in the frontal cortex is more than 200/mm3. In 1985 succeeded the biochemical identification of beta amyloid. But there are more unsolved questions of formation and importance of the plaque formation.
Disease
editAn important criterion of the neuropathological-histological verification of the Alzheimer’s disease is the formation of senile plaques. Beta amyloid peptide associated with senile plaques has been found to play a central role in the risk, onset, and progression of Alzheimer's disease as well. Of particular importance is the long form of beta amyloid, beta amyloid 42. Elevated beta amyloid levels, as well as elevation of the ratio of beta amyloid 42 to the shorter major form beta amyloid 40, has been identified as important in early events in the pathogenesis of Alzheimer's Disease.[9] Other factors in Alzheimer's disease verification include pathological neurofibrillaries, tangles, and atrophic brain with hydrocephalus. The formation and the distribution of the pathological neurofibrillaries have a regularity[8] and allows one to determine the stage of the disease. In combination with the occurrence of a great number of plaques Alzheimer’s disease can be diagnosed with high probability. A correlation between senile plaque presence and Down Syndrome has also been verified.[1]
Research
editAn increasing variety of compounds that reduce beta amyloid levels are being identified, several have beta amyloid 42 selectivity whereas others attempt to modulate amyloid precursor protein. Such compounds are now reaching clinical evaluation to determine how they may be of benefit in the treatment of Alzheimer's disease.[9]
See also
editReferences
edit- ^ a b Cras, P; Kawai, M; Lowery, D; Gonzalez-DeWhitt, P; Greenberg, B; Perry, G (September 1991). "Senile plaque neurites in Alzheimer disease accumulate amyloid precursor protein". Proceedings of the National Academy of Sciences of the United States of America. 88. Clevland, OH: Institute of Pathology: 7552–7556. PMID PMC52339.
{{cite journal}}: Check|pmid=value (help); Cite has empty unknown parameters:|lay-date=and|lay-source=(help); More than one of|author=and|last1=specified (help)CS1 maint: date and year (link) - ^ a b Ksiezak-Reding, H; Morgan, K; Mattiace, LA; Davies, P; Liu, WK; Yen, SH; Weidenheim, K; Dickson, DW (1994). "Ultrastructure and biochemical composition of paired helical filaments in corticobasal degeneration" [Ultrastructure and biochemical composition of paired helical filaments in corticobasal degeneration.]. American Journal of Pathology. 145 (6): 1496–508. PMC 1887493. PMID 7992852.
{{cite journal}}: Cite has empty unknown parameters:|lay-date=and|lay-source=(help) - ^ a b Franke, M (1976). "Statistische Untersuchungen über die senilen Drusen im menschlichen Gehirn / Thesen". Berlin, Germany: Neuropathologische Abteilung.
- ^ Lamy, C; Duyckaerts, C; Delaere, P; Payan, C; Fermanian, J; Poulain, V; Hauw, JJ (November–December 1989). "Comparison of seven staining methods for senile plaques and neurofibrillary tangles in a prospective series of 15 elderly patients". Neuropathology and Applied Neurobiology. 15 (6). Paris, France: Laboratoire de Neuropathologie: 563–578. doi:10.1111/j.1365-2990.1989.tb01255.x. PMID 2482455.
{{cite journal}}: Cite has empty unknown parameters:|lay-date=and|lay-source=(help)CS1 maint: date and year (link) CS1 maint: date format (link) - ^ Mavrogiorgou, P; Gertz, HJ; Ferszt, R; Wolf, R; Bar, KJ; Juckel, G (December 2011). "Are routine methods good enough to stain senile plaques and neurofibrillary tangles in different brain regions of demented patients?". Psychiatria Danubina. 23 (4). Bochum, Germany: 334–339. PMID 22075733.
{{cite journal}}: Cite has empty unknown parameters:|lay-date=and|lay-source=(help)CS1 maint: date and year (link) - ^ a b Suh, YH; Checler, F (September 2002). "Amyloid precursor protein, presenilins, and alpha-synuclein: molecular pathogenesis and pharmacological applications in Alzheimer's disease". Pharmacological Reviews. 54 (3): 469–525. doi:10.1124/pr.54.3.469. PMID 12223532.
{{cite journal}}: CS1 maint: date and year (link) - ^ Op den Velde, W; Stam, FC (January 1976). "Some cerebral proteins and enzyme systems in Alzheimer's presenile and senile dementia". Journal of the American Geriatrics Society. 1. 24 (1). New York, NY: Blackwell Science: 12–16. doi:10.1111/j.1532-5415.1976.tb03247.x. PMID 1244383.
{{cite journal}}: Cite has empty unknown parameters:|lay-source=and|lay-date=(help)CS1 maint: date and year (link) - ^ a b Braak, H; Braak, E; Bohl, J (1993). "Staging of Alzheimer-related cortical destruction". European Neurology. 33 (6). Frankfurt, Germany: Department of Anatomy, Goethe University: 403–408. doi:10.1159/000116984. PMID 8307060.
{{cite journal}}: Cite has empty unknown parameters:|lay-source=and|lay-date=(help) - ^ a b Findeis, MA (November 2007). "The role of amyloid beta peptide 42 in Alzheimer's disease". Pharmacology & Therapeutics. 2. 116 (2). Boston, MA: Satori Pharmaceuticals Incorporated: 266–286. doi:10.1016/j.pharmthera.2007.06.006. PMID 17716740.
{{cite journal}}: Cite has empty unknown parameters:|lay-source=and|lay-date=(help)CS1 maint: date and year (link)
Further Reading
edit- Jellinger KA. Neurodegenerative Erkrankungen (ZNS) - Eine aktuelle Übersicht.. Journal für Neurologie, Neurochirurgie und Psychiatrie. 2005;6(1):9-18.
- Cruz L, Urbanc B, Buldyrev SV, Christie R, Gomez-Isla T, Havlin S, McNamara M, Stanley HE, Hyman BT. Aggregation and disaggregation of senile plaques in Alzheimer disease. Proceedings of the National Academy of Sciences of the United States of America. 1997;94(14):7612-7616. PMID Expression error: Unrecognized word "pmc"..
- Stone J. What initiates the formation of senile plaques? The origin of Alzheimer-like dementias in capillary haemorrhages.. Medical hypotheses. 2008;71(3):347-359. PMID 18524497.