| Pre-eclampsia | |
|---|---|
| Other names | Preeclampsia toxaemia (PET) |
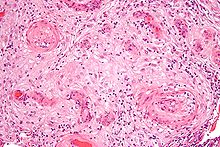 | |
| A micrograph showing hypertrophic decidual vasculopathy, a finding seen in gestational hypertension and pre-eclampsia. H&E stain. | |
| Specialty | Obstetrics |
| Symptoms | High blood pressure, protein in the urine[1] |
| Complications | Red blood cell breakdown, low blood platelet count, impaired liver function, kidney problems, swelling, shortness of breath due to fluid in the lungs, eclampsia[2][3] |
| Usual onset | After 20 weeks of pregnancy[2] |
| Risk factors | Obesity, prior hypertension, older age, diabetes mellitus[2][4] |
| Diagnostic method | BP > 140 mmHg systolic or 90 mmHg diastolic at two separate times[3] |
| Prevention | Aspirin, calcium supplementation, treatment of prior hypertension[4][5] |
| Treatment | Delivery, medications[4] |
| Medication | Labetalol, methyldopa, magnesium sulfate[4][6] |
| Frequency | 2–8% of pregnancies[4] |
| Deaths | 46,900 hypertensive disorders in pregnancy (2015)[7] |
Pre-eclampsia (PE) is a disorder of pregnancy characterized by the onset of high blood pressure and often a significant amount of protein in the urine.[1][8] When it arises, the condition begins after 20 weeks of pregnancy.[2][3] In severe disease there may be red blood cell breakdown, a low blood platelet count, impaired liver function, kidney dysfunction, swelling, shortness of breath due to fluid in the lungs, or visual disturbances.[2][3] Pre-eclampsia increases the risk of poor outcomes for both the mother and the baby.[3] If left untreated, it may result in seizures at which point it is known as eclampsia.[2]
Risk factors for pre-eclampsia include obesity, prior hypertension, older age, and diabetes mellitus.[2][4] It is also more frequent in a woman's first pregnancy and if she is carrying twins.[2] The underlying mechanism involves abnormal formation of blood vessels in the placenta amongst other factors.[2] Most cases are diagnosed before delivery. Rarely, pre-eclampsia may begin in the period after delivery.[3] While historically both high blood pressure and protein in the urine were required to make the diagnosis, some definitions also include those with hypertension and any associated organ dysfunction.[3][9] Blood pressure is defined as high when it is greater than 140 mmHg systolic or 90 mmHg diastolic at two separate times, more than four hours apart in a woman after twenty weeks of pregnancy.[3] Pre-eclampsia is routinely screened for during prenatal care.[10][11]
Recommendations for prevention include: aspirin in those at high risk, calcium supplementation in areas with low intake, and treatment of prior hypertension with medications.[4][5][12] In those with pre-eclampsia delivery of the baby and placenta is an effective treatment.[4] When delivery becomes recommended depends on how severe the pre-eclampsia and how far along in pregnancy a woman is.[4] Blood pressure medication, such as labetalol and methyldopa, may be used to improve the mother's condition before delivery.[6] Magnesium sulfate may be used to prevent eclampsia in those with severe disease.[4] Bedrest and salt intake have not been found to be useful for either treatment or prevention.[3][4]
Pre-eclampsia affects 2–8% of pregnancies worldwide.[4] Hypertensive disorders of pregnancy (which include pre-eclampsia) are one of the most common causes of death due to pregnancy.[6] They resulted in 46,900 deaths in 2015.[7] Pre-eclampsia usually occurs after 32 weeks; however, if it occurs earlier it is associated with worse outcomes.[6] Women who have had pre-eclampsia are at increased risk of heart disease and stroke later in life.[10] The word "eclampsia" is from the Greek term for lightning.[13] The first known description of the condition was by Hippocrates in the 5th century BC.[13]
References edit
- ^ a b Eiland E, Nzerue C, Faulkner M (2012). "Preeclampsia 2012". Journal of Pregnancy. 2012: 586578. doi:10.1155/2012/586578. PMC 3403177. PMID 22848831.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g h i Al-Jameil N, Aziz Khan F, Fareed Khan M, Tabassum H (February 2014). "A brief overview of preeclampsia". Journal of Clinical Medicine Research. 6 (1): 1–7. doi:10.4021/jocmr1682w. PMC 3881982. PMID 24400024.
- ^ a b c d e f g h i American College of Obstetricians Gynecologists; Task Force on Hypertension in Pregnancy (November 2013). "Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy" (PDF). Obstetrics and Gynecology. 122 (5): 1122–31. doi:10.1097/01.AOG.0000437382.03963.88. PMC 1126958. PMID 24150027. Archived from the original (PDF) on 2016-01-06. Retrieved 2020-07-18.
- ^ a b c d e f g h i j k l WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia (PDF). 2011. ISBN 978-92-4-154833-5. Archived (PDF) from the original on 2015-05-13.
- ^ a b Henderson JT, Whitlock EP, O'Connor E, Senger CA, Thompson JH, Rowland MG (May 2014). "Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 160 (10): 695–703. doi:10.7326/M13-2844. PMID 24711050.
- ^ a b c d Arulkumaran N, Lightstone L (December 2013). "Severe pre-eclampsia and hypertensive crises". Best Practice & Research. Clinical Obstetrics & Gynaecology. 27 (6): 877–84. doi:10.1016/j.bpobgyn.2013.07.003. PMID 23962474.
- ^ a b Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ Hypertension in pregnancy. ACOG. 2013. p. 2. ISBN 9781934984284. Archived from the original on 2016-11-18. Retrieved 2016-11-17.
- ^ Lambert G, Brichant JF, Hartstein G, Bonhomme V, Dewandre PY (2014). "Preeclampsia: an update". Acta Anaesthesiologica Belgica. 65 (4): 137–49. PMID 25622379.
- ^ a b Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R (August 2010). "Pre-eclampsia". Lancet. 376 (9741): 631–44. doi:10.1016/S0140-6736(10)60279-6. PMID 20598363.
- ^ Bibbins-Domingo K, Grossman DC, Curry SJ, Barry MJ, Davidson KW, Doubeni CA, et al. (April 2017). "Screening for Preeclampsia: US Preventive Services Task Force Recommendation Statement". JAMA. 317 (16): 1661–1667. doi:10.1001/jama.2017.3439. PMID 28444286.
- ^ US Preventive Services Task, Force.; Davidson, KW; Barry, MJ; Mangione, CM; Cabana, M; Caughey, AB; Davis, EM; Donahue, KE; Doubeni, CA; Kubik, M; Li, L; Ogedegbe, G; Pbert, L; Silverstein, M; Simon, MA; Stevermer, J; Tseng, CW; Wong, JB (28 September 2021). "Aspirin Use to Prevent Preeclampsia and Related Morbidity and Mortality: US Preventive Services Task Force Recommendation Statement". JAMA. 326 (12): 1186–1191. doi:10.1001/jama.2021.14781. PMID 34581729.
- ^ a b Mohler, Emile R. (2006). Advanced Therapy in Hypertension and Vascular Disease. PMPH-USA. pp. 407–408. ISBN 9781550093186. Archived from the original on 2015-10-05.