| Mr. Ibrahem/Heart transplantation | |
|---|---|
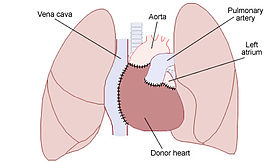 Placement of a donor heart in an orthotopic procedure. Note how the back of the person's left atrium and great vessels are left in place. | |
| Other names | Cardiac transplant, heart transplant |
| Specialty | Cardiothoracic surgery[1] |
| Complications | Rejection, infection, allograft vasculopathy[2] |
| Types | Orthotopic (usual position) Heterotopic (unusual position)[1][3] |
| Frequency | 5,000 per year[4] |
A heart transplantation is major surgery to remove a seriously diseased heart from a person (recipient) and replace it with a normal one from another person (donor).[1] It is performed when, despite other treatments, the heart fails to pump blood effectively such as in end-stage heart failure or severe coronary artery disease.[1] It is generally an option for a young person with severe irreversible heart failure who has a life expectancy of less than 6 months.[2]
Just over half of recipients have non-ischaemic cardiomyopathy, a third have coronary artery disease, and the rest comprise of valvular heart disease, congenital heart disease and re-transplantations.[1] When performed for heart failure, recipients generally have severe limitation of physical activity, while on optimal treatment, and have undergone other appropriate procedures such as cardiac resynchronisation therapy and have an implantable cardioverter-defibrillator.[1] Scoring systems exist to guide suitability of a recipient.[6] Generally, donors have brainstem death (heart-beating donors); though a few centers have programs using donors following circulatory determined death (non-heart beating donors).[1]
It is not safe to perform a heart transplant if there is high pulmonary vascular resistance or an active cancer.[2] Other reasons for not doing the surgery include active infection, severe kidney or liver failure, recent pulmonary embolism, severe lung disease, or diabetes with complications.[1] Having another serious disease with a poor outcome, recent stroke, drug and alcohol misuse, or obesity can also increase risks.[2] In some centers the surgery is only done in people under the age 60 years.[2] Complications include rejection and allograft vasculopathy.[2] The requirement of immunosuppression may increase the risk of infection, particularly in the first year after surgery.[1] Other problems that might occur include high blood pressurre, high cholesterol and cancer, particularly skin cancer.[2] Better results are achieved if the donor heart is placed within 4 hours of its retrieval, and if the recipient is younger.[1]
Most are performed as a single heart transplant, but it may be combined with a lung, liver or kidney transplant.[1] The donor is fully heparinised before the heart is retrieved and placed in cold saline in an insulated organ transport box.[1] The more common method is bi-caval, a type of orthotopic procedure where the donor heart is placed in the same spot as the persons prior heart.[1][3] It involves joining the donor left atrium to the recipients atrial cuff, and then modelling the pulmonary artery and aorta, before releasing the cross-clamp to complete the remaining joins.[1] A heterotopic (“piggy-backed”) procedure may be done to assist left ventricular function, and involves leaving the prior heart in place while joining the donor heart to its right.[3] Heart transplantation can improve the quality and duration of life, particularly in younger recipients.[2][7] As the donor heart has lost its nerve supply, some of its functions are different.[2] It beats faster and loses the normal blood pressure variation though the day.[2]
As of 2020 more than 120,000 heart transplants have been performed since the first in 1967, by South African cardiac surgeon Christiaan Barnard.[1] More than 5,000 heart transplants are performed each year worldwide.[4] More than half are performed in the US.[8] Expected survival after surgery at one year is greater than 90% and at five years is 75%.[2] In transplants carried out between 1992 and 2001, the greatest risk of death is in the first year after the procedure, and the average survival is 11 years.[1] If another heart transplant is repeated at a later date, the risks of death are higher.[1] Globally, organ donation has limited the number of procedures performed.[1]
References edit
- ^ a b c d e f g h i j k l m n o p q r s t Page, Aravinda; Abu-Omar, Abu (2020). "70. Heart transplantation". In Raja, Shahzad G. (ed.). Cardiac Surgery: A Complete Guide. Switzerland: Springer. pp. 639–644. ISBN 978-3-030-24176-6. Archived from the original on 2022-02-14. Retrieved 2022-02-14.
- ^ a b c d e f g h i j k l m n o Bunce, Nicholas H.; Ray, Robin; Patel, Hitesh (2020). "30. Cardiology". In Feather, Adam; Randall, David; Waterhouse, Mona (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. p. 1076. ISBN 978-0-7020-7870-5. Archived from the original on 2022-02-15. Retrieved 2022-02-15.
- ^ a b c Arora, Sonali; Attawar, Sandeep (3 October 2021). "Current Status of Cardiac Transplantation in the 21st Century". Indian Journal of Clinical Cardiology: 263246362110452. doi:10.1177/26324636211045223. ISSN 2632-4636. Archived from the original on 16 February 2022. Retrieved 16 February 2022.
- ^ a b Sai Kiran Bhagra; Stephen Pettit; Jayan Parameshwar (2019), "Cardiac transplantation: indications, eligibility and current outcomes", Heart, 105 (3), British Medical Journal: 252–260, doi:10.1136/heartjnl-2018-313103, PMID 30209127, S2CID 52194404, archived from the original on 2022-01-11, retrieved 2022-01-25
- ^ Jungschleger, JGM; Boldyrev, SY; Kaleda, VI; Dark, JH (January 2018). "Standard orthotopic heart transplantation". Annals of cardiothoracic surgery. 7 (1): 169–171. doi:10.21037/acs.2018.01.18. PMID 29492395.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Mantha, Aditya; Lee, Ramon O.; Wolfson, Aaron M. (1 February 2022). "Patient selection for heart transplant: balancing risk". Current Opinion in Organ Transplantation. 27 (1): 36–44. doi:10.1097/MOT.0000000000000943. ISSN 1531-7013. PMID 34939963. Archived from the original on 14 February 2022. Retrieved 14 February 2022.
- ^ Burch M.; Aurora P. (2004). "Current status of paediatric heart, lung, and heart-lung transplantation". Archives of Disease in Childhood. 89 (4): 386–89. doi:10.1136/adc.2002.017186. PMC 1719883. PMID 15033856.
- ^ Cook JA, Shah KB, Quader MA, et al. (2015). "The total artificial heart". Journal of Thoracic Disease. 7 (12): 2172–80. doi:10.3978/j.issn.2072-1439.2015.10.70. PMC 4703693. PMID 26793338.