| Heart failure | |
|---|---|
| Other names | Chronic heart failure (CHF), congestive cardiac failure (CCF),[1][2][3] decompensatio cordis |
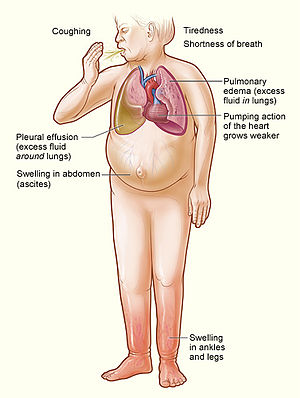 | |
| Signs and symptoms of severe heart failure | |
| Specialty | Cardiology |
| Symptoms | Shortness of breath, feeling tired, leg swelling[4] |
| Duration | Usually lifelong |
| Causes | Heart attack, high blood pressure, abnormal heart rhythm, excessive alcohol use, infection, heart damage[4][5] |
| Risk factors | Smoking, sedentary lifestyle |
| Diagnostic method | Echocardiogram[6] |
| Differential diagnosis | Kidney failure, thyroid disease, liver disease, anemia, obesity[7] |
| Medication | Diuretics, cardiac medications[6][8] |
| Frequency | 40 million (2015),[9] 1–2% of adults (developed countries)[5][10] |
| Deaths | 35% risk of death in first year[4] |
Heart failure (HF), also known as congestive heart failure (CHF) and congestive cardiac failure (CCF), is when the heart is unable to pump sufficiently to maintain blood flow to meet the body's needs.[11][12][13] Signs and symptoms of heart failure commonly include shortness of breath, excessive tiredness, and leg swelling.[4] The shortness of breath is usually worse with exercise or while lying down, and may wake the person at night.[4] A limited ability to exercise is also a common feature.[14] Chest pain, including angina, does not typically occur due to heart failure.[15]
Common causes of heart failure include coronary artery disease, including a previous myocardial infarction (heart attack), high blood pressure, atrial fibrillation, valvular heart disease, excess alcohol use, infection, and cardiomyopathy of an unknown cause.[4][5] These cause heart failure by changing either the structure or the function of the heart.[4] The two types of left ventricular heart failure – heart failure with reduced ejection fraction (HFrEF), and heart failure with preserved ejection fraction (HFpEF) – are based on whether the ability of the left ventricle to contract, or to relax, is affected.[4] The severity of the heart failure is graded by the severity of symptoms with exercise.[7] Heart failure is not the same as heart attack (in which part of the heart muscle dies) or cardiac arrest (in which blood flow stops altogether).[16][17] Other diseases that may have symptoms similar to heart failure include obesity, kidney failure, liver problems, anemia, and thyroid disease.[7] Diagnosis is based on symptoms, physical findings, and echocardiography.[6] Blood tests, electrocardiography, and chest radiography may be useful to determine the underlying cause.[6]
Treatment depends on the severity and cause of the disease.[6] In people with chronic stable mild heart failure, treatment commonly consists of lifestyle modifications such as stopping smoking, physical exercise, and dietary changes, as well as medications.[8][18] In those with heart failure due to left ventricular dysfunction, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, or valsartan/sacubitril along with beta blockers are recommended.[6][19] For those with severe disease, aldosterone antagonists, or hydralazine with a nitrate may be used.[6] Diuretics are useful for preventing fluid retention and the resulting shortness of breath.[8] Sometimes, depending on the cause, an implanted device such as a pacemaker or an implantable cardiac defibrillator (ICD) may be recommended.[6] In some moderate or severe cases, cardiac resynchronization therapy (CRT)[20] or cardiac contractility modulation may be of benefit.[21] A ventricular assist device (for the left, right, or both ventricles), or occasionally a heart transplant may be recommended in those with severe disease that persists despite all other measures.[8]
Heart failure is a common, costly, and potentially fatal condition.[22] In 2015, it affected about 40 million people globally.[9] Overall around 2% of adults have heart failure[22] and in those over the age of 65, this increases to 6–10%.[5][23] Rates are predicted to increase.[22] The risk of death is about 35% the first year after diagnosis, while by the second year the risk of death is less than 10% for those who remain alive.[4] This degree of risk of death is similar to some cancers.[4] In the United Kingdom, the disease is the reason for 5% of emergency hospital admissions.[4] Heart failure has been known since ancient times, with the Ebers papyrus commenting on it around 1550 BCE.[14]
References edit
- ^ "Living Well With Chronic Heart Failure" (PDF). Heart Foundation. p. 18. Archived from the original (PDF) on 22 December 2014. Retrieved 25 May 2014.
- ^ Harrison, Richard N.; Daly, Lynda (2011). A Nurse's Survival Guide to Acute Medical Emergencies. Elsevier Health Sciences. p. 26. ISBN 978-0-7020-4900-2. Archived from the original on 14 June 2020. Retrieved 25 July 2020.
- ^ "Congestive heart failure (CHF)". Archived from the original on 6 April 2016. Retrieved 12 November 2018.
- ^ a b c d e f g h i j k National Clinical Guideline Centre (UK) (August 2010). "Chronic heart failure: National clinical guideline for diagnosis and management in primary and secondary care: Partial update". National Clinical Guideline Centre: 19–24. PMID 22741186.
- ^ a b c d McMurray JJ, Pfeffer MA (2005). "Heart failure". Lancet. 365 (9474): 1877–89. doi:10.1016/S0140-6736(05)66621-4. PMID 15924986.
- ^ a b c d e f g h "Chronic Heart Failure: National Clinical Guideline for Diagnosis and Management in Primary and Secondary Care: Partial Update". National Clinical Guideline Centre: 34–47. Aug 2010. PMID 22741186.
- ^ a b c "Chronic Heart Failure: National Clinical Guideline for Diagnosis and Management in Primary and Secondary Care: Partial Update". National Clinical Guideline Centre: 38–70. Aug 2010. PMID 22741186.
- ^ a b c d "Chronic Heart Failure: National Clinical Guideline for Diagnosis and Management in Primary and Secondary Care: Partial Update". National Clinical Guideline Centre: 71–153. Aug 2010. PMID 22741186.
- ^ a b GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
{{cite journal}}:|author=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. (August 2016). "2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC" (PDF). European Journal of Heart Failure (Review). 18 (8): 891–975. doi:10.1002/ejhf.592. PMID 27207191. Archived (PDF) from the original on 14 June 2020. Retrieved 25 July 2020.
- ^ "heart failure" at Dorland's Medical Dictionary
- ^ "Heart failure". Health Information. Mayo Clinic. 23 December 2009. DS00061. Archived from the original on 13 January 2010.
- ^ "Definition of Heart failure". Medical Dictionary. MedicineNet. 27 April 2011. Archived from the original on 8 December 2011.
- ^ a b McDonagh, Theresa A. (2011). Oxford textbook of heart failure. Oxford: Oxford University Press. p. 3. ISBN 978-0-19-957772-9. Archived from the original on 29 July 2020. Retrieved 25 July 2020.
- ^ O'Connor, Christopher M. (2005). Managing Acute Decompensated Heart Failure a Clinician's Guide to Diagnosis and Treatment. London: Informa Healthcare. p. 572. ISBN 978-0-203-42134-5. Archived from the original on 29 July 2020. Retrieved 25 July 2020.
- ^ Willard & Spackman's occupational therapy. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. 2014. p. 1124. ISBN 978-1-4511-1080-7. Archived from the original on 29 July 2020. Retrieved 25 July 2020.
- ^ The Cardiac Care Unit Survival Guide. Lippincott Williams & Wilkins. 2012. p. 98. ISBN 978-1-4511-7746-6. Archived from the original on 29 July 2020. Retrieved 25 July 2020.
- ^ Long L, Mordi IR, Bridges C, Sagar VA, Davies EJ, Coats AJ, et al. (January 2019). "Exercise-based cardiac rehabilitation for adults with heart failure". The Cochrane Database of Systematic Reviews. 1: CD003331. doi:10.1002/14651858.CD003331.pub5. PMC 6492482. PMID 30695817.
- ^ Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Colvin MM, et al. (September 2016). "2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America". Circulation. 134 (13): e282–93. doi:10.1161/CIR.0000000000000435. PMID 27208050.
- ^ Tracy CM, Epstein AE, Darbar D, DiMarco JP, Dunbar SB, Estes NA, et al. (October 2012). "2012 ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. [corrected]". Circulation. 126 (14): 1784–800. doi:10.1161/CIR.0b013e3182618569. PMID 22965336.
- ^ Kuck KH, Bordachar P, Borggrefe M, Boriani G, Burri H, Leyva F, et al. (January 2014). "New devices in heart failure: an European Heart Rhythm Association report: developed by the European Heart Rhythm Association; endorsed by the Heart Failure Association". Europace. 16 (1): 109–28. doi:10.1093/europace/eut311. PMID 24265466.
- ^ a b c Metra M, Teerlink JR (October 2017). "Heart failure". Lancet. 390 (10106): 1981–1995. doi:10.1016/S0140-6736(17)31071-1. PMID 28460827.
- ^ Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, et al. (October 2008). "ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM)". European Heart Journal. 29 (19): 2388–442. doi:10.1093/eurheartj/ehn309. PMID 18799522. Also at doi:10.1016/j.ejheart.2008.08.005