Hyperbilirubinemia is a clinical condition referring to an elevation of blood bilirubin level due to the inability to properly metabolize or excrete bilirubin, a product from the breakdown of erythrocytes, and in severe cases is manifested as jaundice, which is yellowing of tissues like skin and the sclera of eyes when excess bilirubin deposits in them.[1] By definition, bilirubin concentration of greater than 3 mg/ml is considered hyperbilirubinemia, following which jaundice progressively develops and becomes clearly visible when plasma levels reach 20 mg/ml.[2]
Rather than a disease itself, hyperbilirubinemia is indicative of multifactorial underlying disorders that can be traced back to deviations from normal bilirubin metabolism.
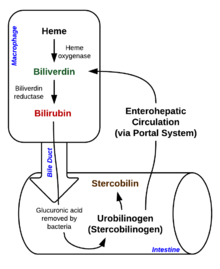
The total average daily production of bilirubin in humans is 4mg/kg. 80% of which is derived from haemoglobin (Hb) upon breakdown of erythrocytes, with the remainder coming from hemp proteins, like myoglobin and cytochrome, turnover.[3] Hb is broken down to globin and haem, which encounters further degradation through a multi-step enzymatic process. [4]. After two sequential reactions converting Hb into bilirubin IX-alpha, this unconjugated bilirubin is released into the bloodstream, where a significant amount binds reversibly with plasma protein albumin and dissociates to be taken up by liver cells through organic anion transport proteins (OATPs) on cell membranes.[1] Inside hepatocytes, bilirubin is conjugated through uridine diphosphate-glucuronosyl-transferase (UGT) to form bilirubin diglucuronide, otherwise termed conjugated bilirubin, which is transported across the plasma membrane by multidrug resistant-associated protein 2 (MRP2) to finally enter bile capillaries.[4] From there, conjugated bilirubin is secreted into the small intestine with bile where a portion is reabsorbed and cycled back to the liver. Unabsorbed bilirubin reaches the colon to be hydrolysed and reduced into urobilinogen, most of which is excreted in faeces.[4]
Hyperbilirubinemia rarely has adverse outcomes. Kernicterus, a type of brain injury caused by unconjugated bilirubin neurotoxicity, occurs only in extreme cases. Adult hyperbilirubinemia, unlike newborn jaundice, does not require therapy.
Diagnosis edit
Classification of hyperbilirubinemia and diagnosis of the underlying disease is crucial for prescribing treatment.[5]
To begin with, physical examination reviews clinical symptoms like degree of jaundice, vital signs and sensations of pain, followed by urine tests, blood analysis and imaging. [2][4] The degree of yellowish staining of the conjunctiva and skin in jaundice is proportional to hyperbilirubinemia to some extent.[5] Vital signs, such as fever, tachycardia and hypotension, suggest hyperbilirubinemia induced by viral hepatitis.[4] Abdominal pain could indicate biliary tract obstruction and cirrhosis.[4]
Urinalysis serves as a first-line diagnostic tool. Conjugated bilirubin, being water-soluble, can be excreted through urine. Hence, dark urine tested bilirubin positive signifies conjugated hyperbilirubinemia.[2]
Serum tests evaluate plasma bilirubin, haemolysis and liver function and are essential for definitive diagnosis. When total serum bilirubin exceeds 2.5 mg/dL and unconjugated bilirubin occupies >85% of total amount, it is classified as unconjugated hyperbilirubinemia.[5] A complete blood cell count illustrating decreased fraction of intact erythrocytes signifies haemolysis which hints for haemolytic diseases.[4] Other than haemolysis, hepatocellular injury indicative of liver diseases like hepatitis can be inferred through increased plasma concentration of aminotransferases AST and ALT, enzyme markers of liver function.[6]
Apart from physical status, medical, drug, family and social history rule out unrelated diseases and give direction to further tests.[2] Reviewing medical history enables screening for causative diseases, such as hepatobiliary diseases, hepatitis and virus infections while drug history reflect toxin exposure and drug use enhancing liver injuries.[4] Intra-family recurrent liver disorders give clues to genetic mutations hence hyperbilirubinemia-associated congenital diseases. Social factors like alcohol intake and sexual history are also considered.[2]
Upon preliminary diagnosis, imaging is ordered to investigate suspected biliary obstruction or liver damage. Right upper quadrant ultrasound is adopted primarily for its high sensitivity and specificity in detecting gallstones and biliary damage.[4] Pancreatic abnormalities are assessed through computed tomography (CT) and magnetic resonance imaging (MRI) whereas liver biopsy is best-suited for intrahepatic diseases.[2][7]
Risk Factors edit
Risk factors of hyperbilirubinemia vary depending on its pathophysiology.
Genetics and external factors also contribute to the disease. Genetic diseases and chemicals that hinder the hepatic uptake of bilirubin, increase the synthetic rate of bilirubin or decrease the bilirubin conjugation rate are risk factors of hyperbilirubinemia.[8] Examples of drugs include rifampin, sulfa drug and ethinyl estradiol respectively.[2]
Alcohol significantly increases risk of hyperbilirubinemia through causing liver damage that hinders bilirubin uptake and bilirubin metabolism. Long term heavy alcohol consumption induces fatty liver and hepatitis, possibly progressing to cirrhosis.[5] As alcohol is degraded, fat globules accumulate in liver tissues and gradually develop into fatty liver. Toxic metabolites of alcohol also injure liver tissues and lead to liver inflammation called hepatitis. Such repeated damage and repair of liver tissues eventually result in cirrhosis, in which functional liver cells are replaced by nonfunctional scar tissues.[9] These conditions, collectively named chronic alcoholic liver diseases, are observed in patients with daily alcohol consumption of 56-70g over 10 years. Meanwhile, acute alcoholic hepatitis may develop with the same amount of daily alcohol intake within 2 hours, inducing acute hyperbilirubinemia.[5][9]
Another risk factor for hyperbilirubinemia is pregnancy. Gallstones are more common in pregnant women due to elevated hormones and cholesterol levels, which block the bile duct and cause hyperbilirubinemia.[10] Besides, preeclampsia and eclampsia, denoted by high blood pressure, are linked to hyperbilirubinemia through damaging highly perfused organs, usually liver and kidneys.[11] Finally, acute fatty liver of pregnancy caused by mitochondrial dysfunction leads to liver insufficiency. [12][13] All three conditions induce hyperbilirubinemia similarly by diminishing liver function and consequently, bilirubin metabolism.
Hepatic viral infection may cause acute and chronic hyperbilirubinemia. Hepatitis A virus causes acute hepatitis but is self-limited.[5] Hepatitis B and C have similar symptoms as hepatitis A in causing acute hepatitis but have later onset only when the stage reaches chronic liver cirrhosis.[5][14] Hepatitis D virus, as a satellite virus, can only infect patients already with hepatitis B thus their complications are similar, only more aggressive.[15] Acute hyperbilirubinemia is found in >70% of hepatitis E patients but chronic infection is infrequent.[16]
The transmission routes of hepatic viruses A and E are oral-faecal while that of hepatic viruses B, C and D are parenteral.[5][15][16] In general, conditions that increase risk of contracting hepatitis viruses include [2][17]
- Eating raw shellfish
- Residing in or travelling to hepatitis-infested areas without being vaccinated
- Sharing needles
- Working in healthcare
Pathophysiology edit
Hyperbilirubinemia is classified into unconjugated and conjugated hyperbilirubinemia. The former, referring to elevated unconjugated bilirubin, is often caused by haemolytic diseases resulting in increased bilirubin production and disorders of impaired bilirubin conjugation. The latter is often attributed to direct hepatocyte injury that impedes conjugated bilirubin secretion.[5] The underlying conditions of hyperbilirubinemia can be prehepatic, intrahepatic or post-hepatic.
Prehepatic Causes edit
Unconjugated hyperbilirubinemia arising before bilirubin reaches the liver results from derailment of liver bilirubin conjugation when conjugation capacities are overwhelmed in haemolytic anemias where red blood cells are disproportionately destroyed, leading to excessive haeme metabolism thus bilirubin production.[5] This may stem from hereditary spherocytosis, a congenital disease characterized by abnormally sphere-shaped erythrocytes, rendering erythrocytes prone to degradation.[18] Other causes include enzyme irregularities like G6PD deficiency that produce unusually structured haemoglobins.[18]
Apart from erythrocyte disorders, certain drugs bind to albumin competitively, occupying binding sites for bilirubin. For instance, sulfonamides, an antibacterial drug, displaces bilirubin from albumin, increasing free concentration of unconjugated bilirubin.[19]
Intrahepatic Causes edit
Hepatocellular injury can cause unconjugated and conjugated bilirubinemia.
Unconjugated Bilirubinemia edit
Metabolic enzyme disorders hinders conjugation to varying degrees. Gilbert Syndrome, a hereditary disease affecting 5% of the US population, leads to stress-induced mild hyperbilirubinemia.[8] The mutated UGT1 gene produces defective UGT1A1 enzymes crucial for the conjugation process.[20] This pathology is shared by another genetic disorder, Crigler-Najjar syndrome, which is subdivided into two types: type 1 (CN-1) and type 2 (CN-2), with the former, usually more serious form, displaying complete loss of UGT1A1 enzyme activity and the latter only partially affected.[21] Hence, unlike CN-1 with persistent jaundice since birth, CN-2 shows milder symptoms and may escape diagnosis until adulthood.
Conjugated Bilirubinemia edit
Hepatitis, commonly virus or alcohol induced, causes internal liver inflammation that injures hepatocytes and disrupts conjugated bilirubin transport.[5] Among primary hepatotropic viruses, Hepatitis A presents with acute onset of jaundice, usually after the first 2-3 days upon entering the icteric phase while chronic Hepatitis B and C manifest jaundice progressively.[22] As mentioned, chronic alcohol consumption affects bile acid uptake and secretion, causing chronic hyperbilirubinemia in liver diseases like fatty liver and hepatitis while acute alcoholic hepatitis triggers a surge in bilirubin.[5]
Dubin-Johnson syndrome and Rotor's syndrome, both rare hereditary metabolic defects characterized by synthesis of faulty proteins responsible for exporting conjugated bilirubin out of hepatocytes, are responsible for the vast majority of isolated hyperbilirubinemia without additional symptoms.[23] Dubin-Johnson syndrome is associated with ABCC gene mutations, creating insufficient or non-functional MRP2 transporters for excretion of conjugated bilirubin.[24] Rotor syndrome is caused by homozygous SLCO1B1 and SLCO1B3 gene mutations which instructs production of organic anion transporting polypeptide 1B1 and 1B3 (OATP1B1 and OATP1B3) on liver cell membrane mediating uptake of bilirubin glucuronide from plasma for secretion into bile.[25] Innate shortage of MRP2 transporters, OATP1B1 and OATP1B3 in these two diseases lowers efficiency of bilirubin removal, thus inducing hyperbilirubinemia.
Drug-induced cholestasis is an adverse outcome of drug-induced-liver-disease and is a concern for susceptible patients.[26] Mechanisms other than direct hepatocyte injury includes competitive inhibition by drug metabolites, such as troglitazone metabolites, that outcompetes bilirubin for MRP2 transporters for secretion.[27]
Post-hepatic Causes edit
Post-hepatic hyperbilirubinemia touches on problems arising after bilirubin conjugation, including intrinsic or extrinsic obstruction of the biliary tree that impedes excretion of conjugated bilirubin with bile.
Intrinsic Obstruction Of The Duct System edit
Gallstones in the gallbladder, also known as cholelithiasis, are the most common finding and may progress to cholecystitis, inflammation of gallbladder that obstructs bile outflow.[5] Cholelithiasis may also cause infection with symptoms of jaundice, fever and pain, known as Charcot’s triad.[5]
Extrinsic Obstruction Of The Duct System edit
Secondary extra-hepatic disorders involve organs excluding the liver. When a tumour develops at the pancreas head or bile duct, the common bile duct is compressed and opposes bile flow, eventually leading to hyperbilirubinemia.[4] Gallbladder carcinoma displays enlarged liver with Courvoisier's sign, a mass in the right-upper quadrant.[28]
Complications edit
Extremely high levels of unconjugated bilirubin in plasma allows bilirubin to cross the blood-brain-barrier to reach the brain and central nervous system to impart damage. This is known as kernicterus, or bilirubin encephalopathy. Kernicterus in adults is extremely rare but is more prevalent in newborns with underdeveloped blood-brain barriers and lower albumin binding capacities that otherwise buffers excess bilirubin in adults. To date, only 4 such cases have been published [29][30][31], with 3 of them associated with CN-2, the milder form of the syndrome. The risk of developing kernicterus in CN-2 patients increases during physiological stress, such as prolonged fasting or anesthesia.[21] In infants, a bilirubin-albumin molar ratio indicating the extent of bilirubin binding of >0.8 is considered at risk of kernicterus but the indicative value in adults remains unclear [31][32].
Unbound plasma bilirubin past a threshold exerts neurotoxic effects through triggering diversified metabolic cascades, directly causing decreased oxygen consumption and increased apoptosis, or programmed cell death, in neurons or indirectly through release of pro-inflammatory enzymes by glial cells.[33] The primary targets affected are the basal ganglia, brainstem and cerebellum because of tissue binding, bilirubin uptake and differential cell sensitivity to injury [33][34].
As damage brought by kernicterus is irreversible, prophylactic measures must be taken to avoid critically high unbound bilirubin levels, especially when infection, liver injury, and haemolytic disorders are present.[31]
Treatment edit
Unlike neonates, hyperbilirubinemia itself requires no treatment in adults. Instead, treatment varies from the underlying cause.
As mentioned, cholelithiasis is the most common cause of hyperbilirubinemia. Gallstones can be removed using acid or shock wave in litholytic therapy and lithotripsy, respectively. Alternatively, cholecystectomy can remove the gallbladder directly.[35] Removing obstruction from the biliary tree should resume normal bilirubin elimination.
Currently, vaccination is most effective for prevention of hepatitis A while novel antiviral drugs have been developed for hepatitis B and C viruses infections.[14][36] However, hepatitis D and E-targeting therapy is absent. Patients with chimeric conditions of viral or alcoholic hepatitis, liver cirrhosis and liver failure required liver transplantation as a last resort.
References edit
- ^ a b Memon, Naureen; Weinberger, Barry I; Hegyi, Thomas; Aleksunes, Lauren M (2016-03). "Inherited disorders of bilirubin clearance". Pediatric Research. 79 (3): 378–386. doi:10.1038/pr.2015.247. ISSN 0031-3998. PMC 4821713. PMID 26595536.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ a b c d e f g h "Jaundice - Hepatic and Biliary Disorders". MSD Manual Professional Edition. Retrieved 2022-03-29.
- ^ Adamson, John W.; Longo, Dan L. (2014), Kasper, Dennis; Fauci, Anthony; Hauser, Stephen; Longo, Dan (eds.), "Anemia and Polycythemia", Harrison's Principles of Internal Medicine (19 ed.), New York, NY: McGraw-Hill Education, retrieved 2022-03-29
- ^ a b c d e f g h i j Sullivan, Jeremy I.; Rockey, Don C. (2017-05). "Diagnosis and evaluation of hyperbilirubinemia". Current Opinion in Gastroenterology. 33 (3): 164–170. doi:10.1097/MOG.0000000000000354. ISSN 0267-1379.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d e f g h i j k l m n Roche, Sean P.; Kobos, Rebecca (2004-01-15). "Jaundice in the adult patient". American Family Physician. 69 (2): 299–304. ISSN 0002-838X. PMID 14765767.
- ^ Limdi, J K (2003-06-01). "Evaluation of abnormal liver function tests". Postgraduate Medical Journal. 79 (932): 307–312. doi:10.1136/pmj.79.932.307. ISSN 0032-5473. PMC 1742736. PMID 12840117.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Barry, Kathleen (2018-03-15). "Chronic Pancreatitis: Diagnosis and Treatment". American Family Physician. 97 (6): 385–393. ISSN 1532-0650. PMID 29671537.
- ^ a b VanWagner, Lisa B.; Green, Richard M. (2015-02-03). "Evaluating Elevated Bilirubin Levels in Asymptomatic Adults". JAMA. 313 (5): 516. doi:10.1001/jama.2014.12835. ISSN 0098-7484. PMC 4424929. PMID 25647209.
{{cite journal}}: CS1 maint: PMC format (link) - ^ a b Osna, Natalia A.; Donohue, Terrence M.; Kharbanda, Kusum K. (2017). "Alcoholic Liver Disease: Pathogenesis and Current Management". Alcohol Research: Current Reviews. 38 (2): 147–161. ISSN 2169-4796. PMC 5513682. PMID 28988570.
- ^ Celaj, Stela; Kourkoumpetis, Themistoklis (2021-06-15). "Gallstones in Pregnancy". JAMA. 325 (23): 2410. doi:10.1001/jama.2021.4502. ISSN 0098-7484.
- ^ Duraiswamy, Sangeethapriya; Sheffield, Jeanne S.; Mcintire, Donald; Leveno, Kenneth; Mayo, Marlyn J. (2017-02). "Updated Etiology and Significance of Elevated Bilirubin During Pregnancy: Changes Parallel Shift in Demographics and Vaccination Status". Digestive Diseases and Sciences. 62 (2): 517–525. doi:10.1007/s10620-016-4282-3. ISSN 0163-2116.
{{cite journal}}: Check date values in:|date=(help) - ^ Duraiswamy, Sangeethapriya; Sheffield, Jeanne S.; Mcintire, Donald; Leveno, Kenneth; Mayo, Marlyn J. (2017-02). "Updated Etiology and Significance of Elevated Bilirubin During Pregnancy: Changes Parallel Shift in Demographics and Vaccination Status". Digestive Diseases and Sciences. 62 (2): 517–525. doi:10.1007/s10620-016-4282-3. ISSN 0163-2116.
{{cite journal}}: Check date values in:|date=(help) - ^ Nelson, David B.; Byrne, John J.; Cunningham, F. Gary (2020-03). "Acute Fatty Liver of Pregnancy". Clinical Obstetrics & Gynecology. 63 (1): 152–164. doi:10.1097/GRF.0000000000000494. ISSN 0009-9201.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Thuener, Jennifer (2017-12). "Hepatitis A and B Infections". Primary Care: Clinics in Office Practice. 44 (4): 621–629. doi:10.1016/j.pop.2017.07.005.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Mentha, Nathalie; Clément, Sophie; Negro, Francesco; Alfaiate, Dulce (2019-05). "A review on hepatitis D: From virology to new therapies". Journal of Advanced Research. 17: 3–15. doi:10.1016/j.jare.2019.03.009. PMC 6526199. PMID 31193285.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ a b Kamar, Nassim; Dalton, Harry R.; Abravanel, Florence; Izopet, Jacques (2014-01). "Hepatitis E Virus Infection". Clinical Microbiology Reviews. 27 (1): 116–138. doi:10.1128/CMR.00057-13. ISSN 0893-8512. PMC 3910910. PMID 24396139.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Gheorghe, Liana; Csiki, Irma E.; Iacob, Speranta; Gheorghe, Cristian (2013-01). "The prevalence and risk factors of hepatitis B virus infection in an adult population in Romania: a nationwide survey". European Journal of Gastroenterology & Hepatology. 25 (1): 56–64. doi:10.1097/MEG.0b013e328358b0bb. ISSN 0954-691X.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Phillips, James; Henderson, Adam C. (2018-09-15). "Hemolytic Anemia: Evaluation and Differential Diagnosis". American Family Physician. 98 (6): 354–361. ISSN 1532-0650. PMID 30215915.
- ^ Roy-Chowdhury, Jayanta; Roy-Chowdhury, Namita (2012-01-01), Boyer, Thomas D.; Manns, Michael P.; Sanyal, Arun J. (eds.), "Chapter 62 - Bilirubin Metabolism and Its Disorders", Zakim and Boyer's Hepatology (Sixth Edition), Saint Louis: W.B. Saunders, pp. 1079–1109, doi:10.1016/b978-1-4377-0881-3.00062-0, ISBN 978-1-4377-0881-3, retrieved 2022-03-29
- ^ "Gilbert Syndrome". NORD (National Organization for Rare Disorders). Retrieved 2022-03-29.
- ^ a b Bhandari, Jenish; Thada, Pawan K.; Yadav, Deepak (2022), "Crigler Najjar Syndrome", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 32965842, retrieved 2022-03-29
- ^ Koff, Raymond S. (1992). "Clinical manifestations and diagnosis of hepatitis A virus infection". Vaccine. 10: S15–S17. doi:10.1016/0264-410X(92)90533-P.
- ^ Talaga, Zachary J.; Vaidya, Prabhakar N. (2022), "Dubin Johnson Syndrome", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30725679, retrieved 2022-03-29
- ^ Nies, Anne T.; Keppler, Dietrich (2007-01-29). "The apical conjugate efflux pump ABCC2 (MRP2)". Pflügers Archiv - European Journal of Physiology. 453 (5): 643–659. doi:10.1007/s00424-006-0109-y. ISSN 0031-6768.
- ^ Kumar, Anila; Mehta, Dhruv (2022), "Rotor Syndrome", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30335339, retrieved 2022-03-29
- ^ Lammert, Craig; Bjornsson, Einar; Niklasson, Anna; Chalasani, Naga (2010-02). "Oral medications with significant hepatic metabolism at higher risk for hepatic adverse events". Hepatology. 51 (2): 615–620. doi:10.1002/hep.23317.
{{cite journal}}: Check date values in:|date=(help) - ^ Padda, Manmeet S.; Sanchez, Mayra; Akhtar, Abbasi J.; Boyer, James L. (2011-04). "Drug-induced cholestasis". Hepatology. 53 (4): 1377–1387. doi:10.1002/hep.24229. PMC 3089004. PMID 21480339.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Gore, Richard M. (2007). "Biliary tract neoplasms: diagnosis and staging". Cancer Imaging. 7 (Special Issue A): S15–S23. doi:10.1102/1470-7330.2007.9016. ISSN 1470-7330. PMC 2727973. PMID 17921093.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Waser, Marco; Kleihues, Paul; Frick, Paul (1986-06). "Kernicterus in an adult". Annals of Neurology. 19 (6): 595–598. doi:10.1002/ana.410190614. ISSN 0364-5134.
{{cite journal}}: Check date values in:|date=(help) - ^ Chalasani, N; Chowdhury, Nr; Chowdhury, Jr; Boyer, Td (1997-06). "Kernicterus in an adult who is heterozygous for Crigler-Najjar syndrome and homozygous for Gilbert-type genetic defect". Gastroenterology. 112 (6): 2099–2103. doi:10.1053/gast.1997.v112.pm9178703.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c Bai, Jie; Li, Lu; Liu, Hui; Liu, Shuang; Bai, Li; Song, Wenyan; Chen, Yu; Zheng, Sujun; Duan, Zhongping (2021-03-11). "UGT1A1-related Bilirubin Encephalopathy/Kernicterus in Adults". Journal of Clinical and Translational Hepatology. 000 (000): 000–000. doi:10.14218/JCTH.2020.00108. ISSN 2225-0719. PMC 8111108. PMID 34007799.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Wallenstein, Matthew B.; Bhutani, Vinod K. (2013-12). "Jaundice and Kernicterus in the Moderately Preterm Infant". Clinics in Perinatology. 40 (4): 679–688. doi:10.1016/j.clp.2013.07.007.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Watchko, Jon F.; Tiribelli, Claudio (2013-11-21). Ingelfinger, Julie R. (ed.). "Bilirubin-Induced Neurologic Damage — Mechanisms and Management Approaches". New England Journal of Medicine. 369 (21): 2021–2030. doi:10.1056/NEJMra1308124. ISSN 0028-4793.
- ^ Fernandes, Adelaide; Falcão, Ana Sofia; Abranches, Elsa; Bekman, Evguenia; Henrique, Domingos; Lanier, Lorene M.; Brites, Dora (2009-08). "Bilirubin as a determinant for altered neurogenesis, neuritogenesis, and synaptogenesis". Developmental Neurobiology. 69 (9): 568–582. doi:10.1002/dneu.20727. PMC 2795766. PMID 19449315.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Reshetnyak, Vasiliy Ivanovich (2012). "Concept of the pathogenesis and treatment of cholelithiasis". World Journal of Hepatology. 4 (2): 18. doi:10.4254/wjh.v4.i2.18. ISSN 1948-5182. PMC 3295849. PMID 22400083.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ Castaneda, Daniel; Gonzalez, Adalberto Jose; Alomari, Mohammad; Tandon, Kanwarpreet; Zervos, Xaralambos Bobby (2021-04-28). "From hepatitis A to E: A critical review of viral hepatitis". World Journal of Gastroenterology. 27 (16): 1691–1715. doi:10.3748/wjg.v27.i16.1691. ISSN 1007-9327. PMC 8072198. PMID 33967551.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link)
