Idiopathic hypercalciuria (IH) can be described as an excessive urinary calcium level with normal blood calcium levels, resulting from no apparent underlying cause [1]. IH has become the most common cause of hypercalciuria and is the most significant metabolic risk factor for developing nephrolithiasis or kidney stones [1] . On top of nephrolithiasis, IH predisposes individuals to numerous conditions, primarily osteopenia or osteoporosis [2]. IH is a condition affecting the entire body, generally arising from faulty calcium homeostasis. Calcium homeostasis is a closely monitored process in which slight deviations in calcium transport in the intestines, blood, and bone can easily usher to excessive calcium excretion, bone mineral density loss, or kidney stone formation [1]. Among nephrolithiasis patients, 50%-60% suffer from IH and, on average, have 5%-15% lower bone density than those who do not [3].

The standard definition of hypercalciuria is varied. Hodkinson and Pyrah proposed it be defined as a calcium excretion of over 7.5 mmol in men and 6.25 mmol in women, every 24 hours [4]. Others argue that these values are too restrictive and ignore age, weight considerations, and renal function. Calcium excretion is negatively associated with age until the ages of 30-60, where it increases, then decreases following age 60 [4]. IH can be further clinically considered a daily urinary excretion of >4mg of calcium per kg of body weight [3]. Utilizing this definition is more applicable among different age groups and weight classes.
IH shares many similarities with hyperparathyroidism, a condition associated with the elevated release of parathyroid hormones from the parathyroid glands [5]. The only discernable feature between the two is the normal blood calcium level associated with IH.
Signs and symptoms edit
IH can be presented with many urinary associated signs and symptoms mostly seen in children. They include [6] [7]:
- Urinary incontinence, pollakiuria, and nocturnal enuresis
- Kidney stones and lithiasis
- Urinary Tract Infection (UTI)
- Hematuria, sterile leukocyturia and discrete proteinuria
- Dysuria and chronic abdominal pain
Causes edit
Due to the nature of the condition being idiopathic, meaning the disease cannot be attributed to an immediate cause, there is speculation regarding possible etiologies of IH. It has been hypothesized that there are primarily three mechanisms contributing to IH: increased intestinal calcium absorption, faulty calcium reabsorption in the renal tubules in the kidneys, and an increased rate of bone resorption [8]. Others estimate IH may arise due to excessive expression of vitamin D receptors, known as VDR, or a deficiency in enzymes within the renal tubules [8].
Increased intestinal calcium absorption edit
A study found that patients with idiopathic hypercalciuria have a rate of calcium absorption two times that of healthy individuals and have elevated levels of calcitriol [8]. Calcium is absorbed through intestinal walls, majorly in the duodenum and to lesser extents in the small intestines and the colon, via two transport systems, a vitamin dependent mechanism and a vitamin independent mechanism [9]. Within the vitamin-dependent mechanism, 1, 25 Dihydroxyvitamin D is responsible for increasing intestinal calcium absorption, which was found elevated in certain IH patients, yet remained normal or elevated in others, suggesting other factors resulted in the increased calcium absorption [8]. Instead, the increased expression of VDR in the intestinal walls may result in this [8].
Faulty calcium reabsorption in the renal tubules edit
Another stipulated cause was that our kidneys failed to reabsorb sufficient calcium in the renal tubules. The renal tubules play a crucial role in the reabsorption of substances, including glucose, sodium, and chloride. About 60% of the calcium filtered out by the glomerulus is reabsorbed in the proximal tubules, compared to 25% in the thick ascending limb of the loop of Henle [10]. After the proximal tubules, the distal convoluted tubule and the collecting duct monitor the reabsorption of the remaining calcium. Significantly low levels of calcium reabsorption were found in patients with hypercalciuria [8], suggesting a modification or defect is present in one of the absorptive pathways used by the renal tubules. This effect is hypothesized to arise due to less parathyroid hormone release, a key regulator in maintaining calcium reabsorption, or renal tubule enzyme deficiency, believed to affect the ascending portion of the loop of Henle and the distal tubule. However, the exact enzyme remains unknown [8].
Increased rate of bone resorption edit
It was found that IH patients had lower done density, suggesting increased bone resorption [11]. Bone resorption involves breaking down bone tissue and transferring calcium ions from the bone tissue to the blood [12]. Bone resorption is carried out by specialized bone cells known as osteoclasts [12]. An increase in osteoclast activity can thus lead to hypercalciuria. Histomorphometry studies, however, failed to discover a significant difference in bone volume in IH patients. However, bone formation was reduced [8]. Information regarding the rate of bone resorption clashes between numerous studies.
The mechanism behind how hypercalciuria causes increased bone resorption is still conflicting. A high animal protein diet causes increased bone resorption, causing an increase in bone loss rate [8]. The high level of calcitriol found in hypercalciuria patients mentioned earlier stimulates increased rates of bone resorption and decreases bone formation [8]. Unrestrained amounts of interleukin-1, TNF-α, and GM-CSF released from monocytes, were found in hypercalciuria patients, which are key determinants in bone remodeling efficiency, furthering bone density loss [8].
Diagnosis edit
Diagnosis for IH includes differential diagnosis and diagnostic methods. Differential diagnosis is made to exclude conditions that can contribute to the increased urinary calcium levels and look for apparent causes through an interview, physical examination, and dietary recall. Diagnostic methods are done to measure protein and calcium levels. Proteinuria can be measured with a urine dipstick test. Three different tests may be used to measure calcium levels in urine, namely, 24-hour urine tests, blood tests, and genetic tests. Another measurement for calcium levels is using an oral calcium tolerance test [13]. Furthermore, ultrasound and CT scans of the urinary tract can be done to diagnose kidney stones or kidney abnormalities as IH often accompanies it.
Urine test edit
Since hypercalciuria is believed to be the most common risk factor for calcium nephrolithiasis (CaNL) [3], urine tests are routinely done to analyze the composition of urine. In urine tests, the patient is first given a week of restricted calcium diet. Then, urine samples are collected for two days to assay calcium in the urine. Urine tests with hypercalciuria should result in a 0.2 mg/mg ratio between calcium and creatinine. If calcium excreted in urine is measured to be lower than 0.07 mmol/kg after 24 hours, diet-dependent hypercalciuria can be deduced, and sodium levels in urine can confirm the result. If the test results come back standard but hypercalciuria continues, the patient is diagnosed with IH [8].
Blood tests edit
Since children diagnosed with hematuria are usually also tested for hypercalciuria [14], blood tests in urine are performed to rule out diseases, such as hematuria that may be underlying the cause of hypercalciuria [15].
Genetic tests edit
IH is a complex polygenic disease with an interplay between genetic and environmental factors. Various genetic studies such as genome-wide linkage analysis can be done to search for the genes causing IH. A few genes that may be associated with IH were selected for genetic screening. Such genes include VDR, TRPV5, CasR, and NPT2a [16]. IH is also associated with many monogenic disorders whether or not renal calcification is involved. The most-studied disease is Dent's disease, which is caused by a mutation in CLCN5 or OCRL1 genes. However, IH patients have not been detected to carry the CLCN5 mutation [17].
Treatment edit
The objective of treating IH lies in preventing nephrolithiasis or the formation of kidney stones,suppose blood calcium levels are normal, which can rule out hyperparathyroidism. This can be achieved by adopting a diet of ~800mg of daily calcium, low salt intake, restricted animal protein intake, and increased net fluid intake [8]. It is important to note that a deficient calcium intake diet accompanies the risk of excessive bone loss and can prompt the increased absorption of dietary oxalates, found in many leafy greens and vegetables, which ordinarily combine with calcium in the intestines [18], leading to the formation of oxalate kidney stones [8]. The diet's effectiveness can be determined by repeating a 24-hour urine test.
If hypercalciuria remains present, pharmaceutical interventions are needed, primarily thiazide diuretics [8]. Thiazide therapy has proven effective in preventing the formation of calcium kidney stones, reducing urinary calcium by 30%, and preventing the periodic occurrence of nephrolithiasis [8]. Thiazides are also inclined to lessen urinary citrate excretion and blood potassium levels, making it recommended to prescribe potassium citrate alongside thiazide therapy [3]. A thiazide therapy option includes Hydrochlorothiazide [2]. A study found that hydrochlorothiazide cleared hypercalciuria and increased spine and hip bone density [2]. Another option would be to use chlorthalidone or indapamide [2].
Pharmaceutical interventions should only be made an option succeeding various months following diet therapy, and a low sodium diet must be maintained throughout the use of thiazide diuretics [3]. If Thiazide therapy fails even after combining it with an appropriate diet, oral orthophosphates are the final recommended treatment [3].
Complications edit
If left untreated, hypercalciuria can cause the following complications:
Nephrolithiasis edit
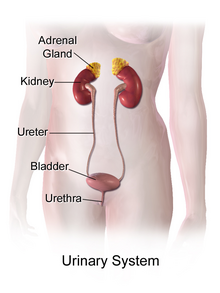
Nephrolithiasis refers to the medical term employing kidney stone formation. The supersaturation of urine with calcium causes an increase in stone formation within the kidneys, as the excess calcium precipitates and begins to form crystals, which develop into larger stones [19]. The stones form in the kidneys and leave the body through the urethra, which can cause tremendous amounts of pain [19].
Osteopenia or Osteoporosis edit
The increased rate of bone resorption causing higher serum calcium levels could lead to osteopenia, or the most severe progression of osteoporosis, in which bones are excessively thin, to the point they fracture easily [20]. Increased fracture risk was identified in nephrolithiasis patients, yet no data directly condemns hypercalciuria for this discovery [20]. Bone loss is, for the most part, unique to nephroliths patients with IH, proposing it has an unidentified role in the increased bone fragility and fracture risk in these patients [20].
Recurrent urinary tract infections (UTI) edit
IH is a significant risk factor for developing UTIs throughout a patient's lifespan. IH does this by impairing the function of the uroepithelium, which acts as our body's defense mechanism against bacteria, by coordinating the inflammatory response and the release of antibodies [21]. The uroepithelium must contact the bacteria to initiate the defense mechanism, but the calcium-oxalate crystals formed in IH prevent this contact, preventing the elimination of bacteria by excretion [21].
Risk Factors edit
Calcium levels in the urine can be affected by multiple systems in the body. These systems include the digestive systems, endocrine systems, and bones. Hence, the various systems at work regulating calcium levels lead to many possible risk factors for IH, although most IH cases have no one direct cause.
One risk factor for IH is excessive vitamin D in the diet or taking medicines which disrupts the calcium regulating mechanisms. Such medications may include furosemide which enhances calcium excreted by urine [22], corticosteroids which reduce the body's ability to absorb calcium [23], and methylxanthines, which stimulate calcium transportation [24]. An example of a methylxanthine is theophylline.
Excessive vitamin D intake can lead to an overexpression of vitamin D receptor (VDR), hence, an elevated serum level of 1,25-dihydroxyvitamin D3 [1,25(OH)2D3], also called calcitriol. An elevated level of 1,25-dihydroxyvitamin D3 then stimulates more absorption of calcium in the intestines [25].
Similarly, a diet high in sodium [26] and protein further increases the risk of having IH [27]. Excessive protein intake may be associated with an enlarged kidney and hence the overproduction of calcitriol that acts on calcium absorption and the increased excretion of calcium in the urine [1].
Another risk factor for IH is insufficient water or fluid intake. Lowered water concentration leads to a higher concentration of CaOx and CaP [19]. Hence, this supersaturation process leads to higher calcium excreted through urine.
Genetic link edit
IH has been considered a multifactorial disorder affected by environmental and genetic factors and has heterogeneous pathogenesis [4]. It also varies according to family characteristics, and a familial distribution of calcium excretion and hypercalciuria has been observed.
Coe et al.'s study discovered that 43% of first-degree relatives and 36% of second degree relatives of patients with hypercalciuria among nine families had IH [28]. It was believed to have an autosomal dominant transmission pattern, as it was not correlated with gender and was observed in all generations [4]. Pak et al. and Nicolaidou et al. identified the same pattern as the one in the study above [29] [30]. Additionally, different hypercalciuria forms within a family were discovered in Lerolle et al., confirming an autosomal dominant transmission [31].
- ^ a b c d Liebman, Scott E.; Taylor, Jeremy G.; Bushinsky, David A. (2006-02-01). "Idiopathic hypercalciuria". Current Rheumatology Reports. 8 (1): 70–75. doi:10.1007/s11926-006-0029-z. ISSN 1534-6307.
- ^ a b c d Adams, John S.; Song, Cindy F.; Kantorovich, Vitaly (1999-04-20). "Rapid Recovery of Bone Mass in Hypercalciuric, Osteoporotic Men Treated with Hydrochlorothiazide". Annals of Internal Medicine. 130 (8): 658–660. doi:10.7326/0003-4819-130-8-199904200-00012. ISSN 0003-4819.
- ^ a b c d e f Leslie, Stephen W.; Sajjad, Hussain (2022), "Hypercalciuria", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 28846247, retrieved 2022-03-28
- ^ a b c d Vezzoli, Giuseppe; Soldati, Laura; Gambaro, Giovanni (2008-05-01). "Update on Primary Hypercalciuria From a Genetic Perspective". Journal of Urology. 179 (5): 1676–1682. doi:10.1016/j.juro.2008.01.011.
- ^ Halabé, A.; Sutton, R. A. (1987). "Primary hyperparathyroidism and idiopathic hypercalciuria". Mineral and Electrolyte Metabolism. 13 (4): 235–241. ISSN 0378-0392. PMID 3306315.
- ^ Penido, Maria Goretti M. G.; Diniz, José S.S.; Moreira, Maria Lúcia S. F.; Tupinambá, Ana L. F.; França, Anderson; Andrade, Bruno H.; Souto, Marcelo F. de O. (2001-03-15). "Idiopathic hypercalciuria: presentation of 471 cases". Jornal de Pediatria. 77 (2): 101–4. doi:10.2223/jped.184. ISSN 0021-7557.
- ^ Cervera, A.; Corral, M. J.; Gómez Campdera, F. J.; De Lecea, A. M.; Luque, A.; López Gómez, J. M. (1987-03). "Idiopathic Hypercalciuria in Children: Classification, Clinical Manifestations and Outcome". Acta Paediatrica. 76 (2): 271–278. doi:10.1111/j.1651-2227.1987.tb10459.x. ISSN 0803-5253.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c d e f g h i j k l m n o p Audran, Maurice; Legrand, Erick (2000-12). "Hypercalciuria". Joint Bone Spine. 67 (6): 509–515. doi:10.1016/S1297-319X(00)00207-4.
{{cite journal}}: Check date values in:|date=(help) - ^ Bronner, Felix (2002-11-27). "Mechanisms of intestinal calcium absorption". Journal of Cellular Biochemistry. 88 (2): 387–393. doi:10.1002/jcb.10330. ISSN 0730-2312.
- ^ Downie, Mallory L; Alexander, R. Todd (2021-04-01). "Molecular mechanisms altering tubular calcium reabsorption". Pediatric Nephrology. doi:10.1007/s00467-021-05049-0. ISSN 0931-041X.
- ^ Giannini, S; Nobile, M; Dalle Carbonare, L; Lodetti, Mg; Sella, S; Vittadello, G; Minicuci, N; Crepaldi, G (2003-09-01). "Hypercalciuria is a common and important finding in postmenopausal women with osteoporosis". European Journal of Endocrinology. 149 (3): 209–213. doi:10.1530/eje.0.1490209. ISSN 0804-4643.
- ^ a b Teitelbaum, Steven L. (2000-09). "Bone Resorption by Osteoclasts". Science. 289 (5484): 1504–1508. doi:10.1126/science.289.5484.1504. ISSN 0036-8075.
{{cite journal}}: Check date values in:|date=(help) - ^ Broadus, Arthur E.; Dominguez, Manual; Bartter, Frederic C. (1978-10). "Pathophysiological Studies in Idiopathic Hypercalciuria: Use of an Oral Calcium Tolerance Test to Characterize Distinctive Hypercalciuric Subgroups*". The Journal of Clinical Endocrinology & Metabolism. 47 (4): 751–760. doi:10.1210/jcem-47-4-751. ISSN 0021-972X.
{{cite journal}}: Check date values in:|date=(help) - ^ Garcia, Clotilde D. (1991-10-01). "Natural History of Hematuria Associated With Hypercalciuria in Children". Archives of Pediatrics & Adolescent Medicine. 145 (10): 1204. doi:10.1001/archpedi.1991.02160100136039. ISSN 1072-4710.
- ^ Bruder Stapleton, prepared by F.; A Report of The Southwest Pediatric Nephrology Study Group (1990-02). "Idiopathic hypercalciuria: Association with isolated hematuria and risk for urolithiasis in children". Kidney International. 37 (2): 807–811. doi:10.1038/ki.1990.49.
{{cite journal}}: Check date values in:|date=(help) - ^ Worcester, Elaine M.; Coe, Fredric L. (2008-03). "New Insights Into the Pathogenesis of Idiopathic Hypercalciuria". Seminars in Nephrology. 28 (2): 120–132. doi:10.1016/j.semnephrol.2008.01.005. PMC 2362396. PMID 18359393.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Devuyst, Olivier; Thakker, Rajesh V (2010). "Dent's disease". Orphanet Journal of Rare Diseases. 5 (1): 28. doi:10.1186/1750-1172-5-28. ISSN 1750-1172. PMC 2964617. PMID 20946626.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ Massey, Linda K; Roman-Smith, Helen; Sutton, Roger A.L (1993-08). "Effect of dietary oxalate and calcium on urinary oxalate and risk of formation of calcium oxalate kidney stones". Journal of the American Dietetic Association. 93 (8): 901–906. doi:10.1016/0002-8223(93)91530-4.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c Coe, Fredric L.; Worcester, Elaine M.; Evan, Andrew P. (2016-09). "Idiopathic hypercalciuria and formation of calcium renal stones". Nature Reviews Nephrology. 12 (9): 519–533. doi:10.1038/nrneph.2016.101. ISSN 1759-5061. PMC 5837277. PMID 27452364.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ a b c Sella, Stefania; Cattelan, Catia; Realdi, Giuseppe; Giannini, Sandro (2008). "Bone disease in primary hypercalciuria". Clinical Cases in Mineral and Bone Metabolism. 5 (2): 118–126. ISSN 1724-8914. PMC 2781204. PMID 22460993.
- ^ a b Nacaroglu, Hikmet Tekin; Demircin, Gülay; Bülbül, Mehmet; Erdogan, Özlem; Akyüz, Sare Gülfem; Çaltik, Aysun (2013-04). "The Association between Urinary Tract Infection and Idiopathic Hypercalciuria in Children". Renal Failure. 35 (3): 327–332. doi:10.3109/0886022X.2013.764254. ISSN 0886-022X.
{{cite journal}}: Check date values in:|date=(help) - ^ Lee, Chien-Te; Chen, Hung-Chun; Lai, Li-Wen; Yong, Kim-Chong; Lien, Yeong-Hau H. (2007-10). "Effects of furosemide on renal calcium handling". American Journal of Physiology-Renal Physiology. 293 (4): F1231–F1237. doi:10.1152/ajprenal.00038.2007. ISSN 1931-857X.
{{cite journal}}: Check date values in:|date=(help) - ^ Homik, Joanne; Suarez-Almazor, Maria E; Shea, Beverley; Cranney, Ann; Wells, George A; Tugwell, Peter (1998-04-27). Cochrane Musculoskeletal Group (ed.). "Calcium and vitamin D for corticosteroid-induced osteoporosis". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD000952. PMC 7046131. PMID 10796394.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Kopf, Gregory S.; Lewis, Cindy A.; Vacquier, Victor D. (1983-09). "Methylxanthines stimulate calcium transport and inhibit cyclic nucleotide phosphodiesterases in abalone sperm". Developmental Biology. 99 (1): 115–120. doi:10.1016/0012-1606(83)90258-0.
{{cite journal}}: Check date values in:|date=(help) - ^ Favus, Murray J.; Karnauskas, Alexander J.; Parks, Joan H.; Coe, Fredric L. (2004-10). "Peripheral Blood Monocyte Vitamin D Receptor Levels Are Elevated in Patients with Idiopathic Hypercalciuria". The Journal of Clinical Endocrinology & Metabolism. 89 (10): 4937–4943. doi:10.1210/jc.2004-0412. ISSN 0021-972X.
{{cite journal}}: Check date values in:|date=(help) - ^ McParland, B. E.; Goulding, A.; Campbell, A. J. (1989-09-30). "Dietary salt affects biochemical markers of resorption and formation of bone in elderly women". BMJ. 299 (6703): 834–835. doi:10.1136/bmj.299.6703.834-a. ISSN 0959-8138. PMC 1837680. PMID 2510848.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Hess, B; Ackermann, D; Essig, M; Takkinen, R; Jaeger, P (1995-06). "Renal mass and serum calcitriol in male idiopathic calcium renal stone formers: role of protein intake". The Journal of Clinical Endocrinology & Metabolism. 80 (6): 1916–1921. doi:10.1210/jcem.80.6.7775641. ISSN 0021-972X.
{{cite journal}}: Check date values in:|date=(help) - ^ Coe, Fredric L.; Parks, Joan H.; Moore, Eddie S. (1979-02-15). "Familial Idiopathic Hypercalciuria". New England Journal of Medicine. 300 (7): 337–340. doi:10.1056/NEJM197902153000703. ISSN 0028-4793.
- ^ Pak, Charles Y.C.; McGuire, James; Peterson, Roy; Britton, Faye; Harrod, Mary Jo (1981-12). "Familial Absorptive Hypercalciuria in a Large Kindred". Journal of Urology. 126 (6): 717–719. doi:10.1016/S0022-5347(17)54715-1. ISSN 0022-5347.
{{cite journal}}: Check date values in:|date=(help) - ^ Nicolaidou, Polyxeni; Themeli, Sofia; Karpathios, Themistoklis; Georgouli, Helen; Athanassaki, Korina; Xaidara, Athina; Messaritakis, John (1996-03). "Family Pattern of Idiopathic Hypercalciuria and its Subtypes:". The Journal of Urology: 1042–1044. doi:10.1097/00005392-199603000-00074. ISSN 0022-5347.
{{cite journal}}: Check date values in:|date=(help) - ^ Lerolle, Nicolas; Coulet, Florence; Lantz, Brigitte; Paillard, Françoise; Houillier, Pascal; Soubrier, Florent; Gattegno, Bernard; Jeunemaitre, Xavier; Ronco, Pierre; Rondeau, Eric (2001-12-01). "No evidence for point mutations of the calcium‐sensing receptor in familial idiopathic hypercalciuria". Nephrology Dialysis Transplantation. 16 (12): 2317–2322. doi:10.1093/ndt/16.12.2317. ISSN 1460-2385.