| Dengue virus | |
|---|---|
| |
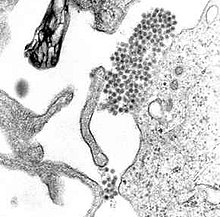
| A TEM micrograph showing Dengue virus virions (the cluster of dark dots near the center). | |
| Virus classification | |
| Group: | Group IV ((+)ssRNA)
|
| Family: | |
| Genus: | |
| Species: | Dengue virus
|
| Justthefacts1/Sandbox |
|---|
Justthefacts1 is testing her Wiki Imp skills by placing random tags on this copied page. Headline attempt edit
,
Dengue fever (pronounced English pronunciation: /ˈdɛŋɡeɪ/, English pronunciation: /ˈdɛŋɡiː/) and dengue hemorrhagic fever (DHF) are acute febrile diseases which occur in the tropics, can be life-threatening[citation needed], and are caused by four closely related virus serotypes of the genus Flavivirus, family Flaviviridae.[1] It is also known as breakbone fever. It occurs widely in the tropics, including northern Argentina, northern Australia, the entirety of Bangladesh, Barbados, Bolivia[2] [failed verification], Brazil, Cambodia, Costa Rica, Dominican Republic,El Salvador,Guatemala, Guyana, Honduras, India, Indonesia, Jamaica, Laos, Malaysia, Mexico, Micronesia, Pakistan, Panama, Paraguay,[3] Philippines, Puerto Rico, Samoa,[4] Singapore, Sri Lanka, Suriname, Taiwan, Thailand, Trinidad, Venezuela and Vietnam, and increasingly in southern China.[5] Unlike malaria, dengue is just as prevalent in the urban districts of its range as in rural areas. Each serotype is sufficiently different that there is no cross-protection and epidemics caused by multiple serotypes (hyperendemicity) can occur. Dengue is transmitted to humans by the Aedes aegypti or more rarely the Aedes albopictus mosquito, which feed during the day.[6]
The WHO says some 2.5 billion people, two fifths of the world's population, are now at risk from dengue and estimates that there may be 50 million cases of dengue infection worldwide every year. The disease is now endemic in more than 100 countries.[7]
Signs and symptoms edit
The disease manifests as a sudden onset of severe headache, muscle and joint pains (myalgias and arthralgias—severe pain that gives it the nickname break-bone fever or bonecrusher disease), fever, and rash.[8] The dengue rash is characteristically bright red petechiae and usually appears first on the lower limbs and the chest; in some patients, it spreads to cover most of the body. There may also be gastritis with some combination of associated abdominal pain, nausea, vomiting, or diarrhea.
Some cases develop much milder symptoms which can be misdiagnosed as influenza or other viral infection when no rash is present. Thus travelers from tropical areas may pass on dengue inadvertently, having not been properly diagnosed at the height of their illness. Patients with dengue can pass on the infection only through mosquitoes or blood products and only while they are still febrile. The classic dengue fever lasts about two to seven days, with a smaller peak of fever at the trailing end of the disease (the so-called "biphasic pattern"). Clinically, the platelet count will drop until the patient's temperature is normal. Cases of DHF also show higher fever, variable hemorrhagic phenomena, thrombocytopenia, and hemoconcentration. A small proportion of cases lead to dengue shock syndrome (DSS) which has a high mortality rate.
Diagnosis edit
The diagnosis of dengue is usually made clinically. The classic picture is high fever with no localising source of infection, a petechial rash with thrombocytopenia and relative leukopenia - low platelet and white blood cell count. Care has to be taken as diagnosis of DHF can mask end stage liver disease and vice versa.
- Fever, bladder problem, constant headaches, eye pain, severe dizziness and loss of appetite.
- Hemorrhagic tendency (positive tourniquet test, spontaneous bruising, bleeding from mucosa, gingiva, injection sites, etc.; vomiting blood, or bloody diarrhea)
- Thrombocytopenia (<100,000 platelets per mm³ or estimated as less than 3 platelets per high power field)
- Evidence of plasma leakage (hematocrit more than 20% higher than expected, or drop in hematocrit of 20% or more from baseline following IV fluid, pleural effusion, ascites, hypoproteinemia)
- Encephalitic occurrences.
Dengue shock syndrome is defined as dengue hemorrhagic fever plus:
- Weak rapid pulse,
- Narrow pulse pressure (less than 20 mm Hg)
- Cold, clammy skin and restlessness.
Dependable, immediate diagnosis of dengue can be performed in rural areas by the use of Rapid Diagnostic Test kits, which also differentiate between primary and secondary dengue infections.[9] Serology and polymerase chain reaction (PCR) studies are available to confirm the diagnosis of dengue if clinically indicated. Dengue can be a life threatening fever.
Cause edit
Dengue fever is caused by Dengue virus (DENV), a mosquito-borne flavivirus. DENV is an ssRNA positive-strand virus of the family Flaviviridae; genus Flavivirus. There are four serotypes of DENV. The virus has a genome of about 11000 bases that codes for three structural proteins, C, prM, E; seven nonstructural proteins, NS1, NS2a, NS2b, NS3, NS4a, NS4b, NS5; and short non-coding regions on both the 5' and 3' ends.[10]
The potential factors causing hemorrhagic fever are varied. The most suspected factors are human's cross-serotypic immune response and membrane fusion process.
Prevention edit
Vaccine development edit
There is no tested and approved vaccine for the dengue flavivirus. There are many ongoing vaccine development programs. Among them is the Pediatric Dengue Vaccine Initiative set up in 2003 with the aim of accelerating the development and introduction of dengue vaccine(s) that are affordable and accessible to poor children in endemic countries.[11] Thai researchers are testing a dengue fever vaccine on 3,000–5,000 human volunteers after having successfully conducted tests on animals and a small group of human volunteers.[12] A number of other vaccine candidates are entering phase I or II testing.[13]
Mosquito control edit
Primary prevention of dengue mainly resides in mosquito control. There are two primary methods: larval control and adult mosquito control.[citation needed] In urban areas, Aedes mosquitos breed on water collections in artificial containers such as plastic cups, used tires, broken bottles, flower pots, etc. Periodic draining or removal of containers is the most effective way of reducing the breeding grounds for mosquitos.[citation needed] Larvicide treatment is another effective way to control the vector larvae, but the larvicide chosen should be long-lasting and preferably have World Health Organization clearance for use in drinking water. There are some very effective insect growth regulators (IGRs) available which are both safe and long-lasting (e.g., pyriproxyfen). For reducing the adult mosquito load, fogging with insecticide is somewhat effective.[citation needed]
Prevention of mosquito bites is another way of preventing disease. This can be achieved by using insect repellent, mosquito traps or mosquito nets.
Mesocyclops edit
In 1998, scientists from the Queensland Institute of Medical Research (QIMR) in Australia and Vietnam's Ministry of Health introduced a scheme that encouraged children to place a water bug, the crustacean Mesocyclops, in water tanks and discarded containers where the Aedes aegypti mosquito was known to thrive.[14] This method is viewed as being more cost-effective and more environmentally friendly than pesticides, though not as effective, and requires the continuing participation of the community.[15]
Even though this method of mosquito control was successful in rural provinces, not much is known about how effective it could be if applied to cities and urban areas. The Mesocyclops can survive and breed in large water containers but would not be able to do so in small containers that most urban dwellers have in their homes. Also, Mesocyclops are hosts for the guinea worm, a pathogen that causes a parasite infection, and so this method of mosquito control cannot be used in countries that are still susceptible to the guinea worm. The biggest dilemma with Mesocyclops is that its success depends on the participation of the community. This idea of a possible parasite-bearing creature in household water containers dissuades people from continuing the process of inoculation and, without the support and work of everyone living in the city, this method will not be successful.[16]
Wolbachia edit
In 2009, scientists from the School of Integrative Biology at The University of Queensland revealed that by infecting Aedes mosquitos with the bacterium Wolbachia, the adult lifespan was reduced by half.[17] In the study, super-fine needles were used to inject 10,000 mosquito embryos with the bacterium. Once an insect was infected, the bacterium would spread via its eggs to the next generation. A pilot release of infected mosquitoes could begin in Vietnam within three years. If no problems are discovered, a full-scale biological attack against the insects could be launched within five years.[18]
Mosquito mapping edit
In 2004, scientists from the Federal University of Minas Gerais, Brazil, discovered a fast way to find and count mosquito population inside urban areas. The technology, named Intelligent Monitoring of Dengue (in Portuguese), uses traps with kairomones that capture Aedes gravid females, and upload insect counts with a combination of cell phone, GPS and internet technology. The result is a complete map of the mosquitoes in urban areas, updated in real time and accessible remotely, that can inform control methodologies.[19] The technology was recognized with a Tech Museum Award in 2006.[20]
Potential antiviral approaches edit
Dengue virus belongs to the family Flaviviridae, which includes the hepatitis C virus, West Nile and Yellow fever viruses among others. Possible laboratory modification of the yellow fever vaccine YF-17D to target the dengue virus via chimeric replacement has been discussed extensively in scientific literature,[21] but as of 2009[update] no full scale studies have been conducted.[22]
In 2006 a group of Argentine scientists discovered the molecular replication mechanism of the virus, which could be specifically attacked by disrupting the viral RNA polymerase.[23] In cell culture[24] and murine experiments[25][26] morpholino antisense oligomers have shown specific activity against Dengue virus.
In 2007 virus replication was attenuated in the laboratory by interfering with activity of the dengue viral protease, and a project to identify drug leads with broad spectrum activity against the related dengue, hepatitis C, West Nile, and yellow fever viruses was launched.[27][28]
Sterile insect technique edit
The sterile insect technique, a form of biological control, has long proved difficult with mosquitos because of the fragility of the males.[29] However, a transgenic strain of Aedes aegypti was announced in 2010 which might alleviate this problem: the strain produces females that are flightless due to a mis-development of their wings,[30] and so can neither mate nor bite. The genetic defect only causes effects in females, so that males can act as silent carriers.[29]
Treatment edit
The mainstay of treatment is timely supportive therapy to tackle shock due to hemoconcentration and bleeding. Close monitoring of vital signs in critical period (between day 2 to day 7 of fever) is critical. Increased oral fluid intake is recommended to prevent dehydration. Supplementation with intravenous fluids may be necessary to prevent dehydration and significant concentration of the blood if the patient is unable to maintain oral intake. A platelet transfusion is indicated in rare cases if the platelet level drops significantly (below 20,000) or if there is significant bleeding. The presence of melena may indicate internal gastrointestinal bleeding requiring platelet and/or red blood cell transfusion.
Aspirin and non-steroidal anti-inflammatory drugs should be avoided as these drugs may worsen the bleeding tendency associated with some of these infections. Patients may receive paracetamol preparations to deal with these symptoms if dengue is suspected.[31]
Research edit
Emerging evidence suggests that mycophenolic acid and ribavirin inhibit dengue replication. Initial experiments showed a fivefold increase in defective viral RNA production by cells treated with each drug.[32] In vivo studies, however, have not yet been done. Unlike HIV therapy, lack of adequate global interest and funding greatly hampers the development of a treatment regime.
At least one distributed computing project (where private computer users can let their computers help find cures) is helping research new dengue drug candidates before they are actually produced. This process saves time and money. See worldcommunitygrid.org The research is public domain and non-profit.
Alternative medicine edit
In Brazilian traditional medicine, cat's claw herb is used to treat patients with dengue.[33] In Philippines, the tawa-tawa herb is used to treat patients with dengue.[34]
Epidemiology edit
| no data < 15 15-30 30-45 45-60 60-75 75-90 | 90-105 105-120 120-135 135-150 150-250 > 250 |
Dengue is transmitted by Aedes mosquitoes, particularly A. aegypti and A. albopictus.
The first recognized Dengue epidemics occurred almost simultaneously in Asia, Africa, and North America in the 1780s, shortly after the identification and naming of the disease in 1779. A pandemic began in Southeast Asia in the 1950s, and by 1975 DHF had become a leading cause of death among children in the region. Epidemic dengue has become more common since the 1980s. By the late 1990s, dengue was the most important mosquito-borne disease affecting humans after malaria, with around 40 million cases of dengue fever and several hundred thousand cases of dengue hemorrhagic fever each year. Significant outbreaks of dengue fever tend to occur every five or six months. The cyclical rise and fall in numbers of dengue cases is thought to be the result of seasonal cycles interacting with a short-lived cross-immunity[clarification needed] for all four strains in people who have had dengue. When the cross-immunity wears off the population is more susceptible to transmission whenever the next seasonal peak occurs. Thus over time there remain large numbers of susceptible people in affected populations despite previous outbreaks due to the four different serotypes of dengue virus and the presence of unexposed individuals from childbirth or immigration.
There is significant evidence, originally suggested by S.B. Halstead in the 1970s, that dengue hemorrhagic fever is more likely to occur in patients who have secondary infections by another one of dengue fever's four serotypes. One model to explain this process is known as antibody-dependent enhancement (ADE), which allows for increased uptake and virion replication during a secondary infection with a different strain. Through an immunological phenomenon, known as original antigenic sin, the immune system is not able to adequately respond to the stronger infection, and the secondary infection becomes far more serious.[35] This process is also known as superinfection.[36][37]
Reported cases of dengue are an under-representation of all cases when accounting for subclinical cases and cases where the patient did not present for medical treatment.
There was a serious outbreak in Rio de Janeiro in February 2002 affecting around one million people and killing sixteen. On March 20, 2008, the secretary of health of the state of Rio de Janeiro, Sérgio Côrtes, announced that 23,555 cases of dengue, including 30 deaths, had been recorded in the state in less than three months. Côrtes said, "I am treating this as an epidemic because the number of cases is extremely high." Federal Minister of Health, José Gomes Temporão also announced that he was forming a panel to respond to the situation. Cesar Maia, mayor of the city of Rio de Janeiro, denied that there was serious cause for concern, saying that the incidence of cases was in fact declining from a peak at the beginning of February.[38] By April 3, 2008, the number of cases reported rose to 55,000 [39]
In Singapore, there are 4,000–5,000 reported cases of dengue fever or dengue haemorrhagic fever every year. In the year 2004, there were seven deaths from dengue shock syndrome.[40]
An epidemic broke out in Bolivia in early 2009, in which 18 people have died and 31,000 infected.
An outbreak of dengue fever was declared in Cairns, located in the tropical north of Queensland, Australia on 1 December 2008. As at 3 March 2009 there were 503 confirmed cases of dengue fever, in a residential population of 152,137. Outbreaks were subsequently declared the neighbouring cities and towns of Townsville (outbreak declared 5 January 2009), Port Douglas (6 February 2009), Yarrabah (19 February 2009), Injinoo (24 February 2009), Innisfail (27 February 2009) and Rockhampton (10 March 2009). There have been occurrences of dengue types one, two, three and four in the region. March 4, 2009, Queensland Health had confirmed an elderly woman had died from dengue fever in Cairns, in the first fatality since the epidemic began last year. The statement said that although the woman had other health problems, she tested positive for dengue and the disease probably contributed to her death.
In 2009, in Argentina, a dengue outbreak was declared the northern provinces of Chaco, Catamarca, Salta, Jujuy, and Corrientes, with over 9673 cases reported as of April 11, 2009 by the Health Ministry [1]. Some travelers from the affected zones have spread the fever as far south as Buenos Aires [2]. Major efforts to control the epidemic in Argentina are focused on preventing its vector (the Aedes mosquitoes) from reproducing. This is addressed by asking people to dry out all possible water reservoirs from where mosquitoes could proliferate (which is, in other countries, known as "descacharrado"). There have also been information campaigns concerning prevention of the dengue fever; and the government is fumigating with insecticide in order to control the mosquito population.[41]
The first cases of dengue fever have recently been reported on the island of Mauritius, in the Indian Ocean. One of the South Asian countries still suffering highly from this problem is Sri Lanka.[42]
Blood transfusion edit
Dengue may also be transmitted via infected blood products (blood transfusions, plasma, and platelets),[43][44] and in countries such as Singapore, where dengue is endemic, the risk was estimated to be between 1.6 and 6 per 10,000 blood transfusions.[45]
History edit
Etymology edit
The origins of the word dengue are not clear, but one theory is that it is derived from the Swahili phrase "Ka-dinga pepo", which describes the disease as being caused by an evil spirit.[46] The Swahili word "dinga" may possibly have its origin in the Spanish word "dengue" meaning fastidious or careful, which would describe the gait of a person suffering the bone pain of dengue fever.[47] Alternatively, the use of the Spanish word may derive from the similar-sounding Swahili.[48]
History of the literature edit
Slaves in the West Indies who contracted dengue were said to have the posture and gait of a dandy, and the disease was known as "Dandy Fever".[49] The first record of a case of probable dengue fever is in a Chinese medical encyclopedia from the Jin Dynasty (265–420 AD) which referred to a “water poison” associated with flying insects.[48] The first confirmed case report dates from 1789 and is by Benjamin Rush, who coined the term "breakbone fever" because of the symptoms of myalgia and arthralgia.[50] The viral etiology and the transmission by mosquitoes were discovered in the 20th century by Sir John Burton Cleland.
Population movements during World War II spread the disease globally. A pandemic of dengue began in Southeast Asia after World War II and has spread around the globe since then.[51]
Society and Culture edit
Use as a biological weapon edit
Dengue fever was one of more than a dozen agents that the United States researched as potential biological weapons before the nation suspended its biological weapons program.[52]
See also edit
- Brazilian research study (in Portuguese) using Cats claw against dengue
- Justthefacts1/Sandbox at Curlie
- Dengue Virus Genomes database search results from the Dengue Virus Database at the Viral Bioinformatics Resource Center
- Discovering Dengue Drugs – Together, a distributed computing project attempting to identify drug leads with broad spectrum activity against dengue.[53]
- Dengue fever in Brazil (slide show, in English and Portuguese)
- Dengue Fever Alliance - Todos Frente al Dengue Alliance to strengthen the capacity of action and management for A World Free of Dengue Fever
References edit
- ^ "Chapter 4, Prevention of Specific Infectious Diseases". CDC Traveler's Health: Yellow Book. Retrieved 2007-05-20.
- ^ "Dengue fever outbreak in Bolivia". BBC. 2009-02-03. Retrieved 2009-02-26.
- ^ Reuters, "Dengue Fever Hits Paraguay", New York Times" (March 4, 2007)
- ^ http://www.samoalivenews.com/Health/Dengue-Fever-Outbreak-Confirmed-In-Samoa.html
- ^ "Zhuhai reports outbreak of dengue fever". China Daily. 200-09-06. Retrieved 2009-11-18.
{{cite web}}: Check date values in:|date=(help) - ^ Dengue Fever – Information Sheet. World Health Organization, October 9, 2006. Retrieved on 2007-11-30.
- ^ Dengue epidemic threatens India's capital
- ^ Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. p. 592. ISBN 0838585299.
{{cite book}}:|author=has generic name (help) - ^ Such a diagnostic kit may consist of a "test cassette" or other device. One type is described as follows: "Dengue fever rapid test devices, also known as one-step dengue tests, are a solid phase immuno-chromatographic assay for the rapid, qualitative and differential detection of dengue IgG and IgM antibodies to dengue fever virus in human serum, plasma or whole blood." Atlas Link Biotech co. Ltd (2008)Dengue Fever Rapid Test Kits. Accessed: 27/06/09. Available at: http://www.ivdpretest.com/Dengue-Rapid-Tests.html
- ^ Hanley, K.A. and Weaver, S.C. (editors) (2010). Frontiers in Dengue Virus Research. Caister Academic Press. ISBN 978-1-904455-50-9.
{{cite book}}:|author=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ "Pediatric Dengue Vaccine Initiative". 2008. Retrieved 2008-10-05.
- ^ "Thailand to test Mahidol-developed dengue vaccine prototype". People's Daily Online. 2005-09-05. Retrieved 2006-10-08.
- ^ Edelman R (July 2007). "Dengue vaccines approach the finish line". Clinical Infectious Diseases. 45 (Suppl 1): S56–60. doi:10.1086/518148. PMID 17582571.
{{cite journal}}: CS1 maint: date and year (link) - ^ Vu SN, Nguyen TY, Kay BH, Marten GG, Reid JW (1 October 1998). "Eradication of Aedes aegypti from a village in Vietnam, using copepods and community participation". Am J Trop Med Hyg. 59 (4): 657–60. doi:10.4269/ajtmh.1998.59.657. PMID 9790448.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Water bug aids dengue fever fight". BBC News. 2005-02-11. Retrieved 2008-10-05.
Kay B, Vu SN (2005). "New strategy against Aedes aegypti in Vietnam". Lancet. 365 (9459): 613–7. doi:10.1016/S0140-6736(05)17913-6. PMID 15708107. - ^ "Control of aedes vectors of dengue in three provinces of Vietnam by use of Mesocyclops (Copepoda) and community-based methods validated by etomology, clinical, and serological surveillance". The American Society of Tropical Medicine and Hygiene. 2002. Retrieved 2009-02-18.
- ^ McMeniman CJ, Lane RV, Cass BN; et al. (January 2009). "Stable Introduction of a Life-Shortening Wolbachia Infection into the Mosquito Aedes aegypti". Science. 323 (5910): 141–4. doi:10.1126/science.1165326. PMID 19119237.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ "Dengue fever breakthrough". Sydney Morning Herald. 2009-01-02. Retrieved 2009-01-02.
- ^ "Dengue fever GPS mapping". CNN.com Technology. 2007-07-09. Retrieved 2009-01-07.
- ^ "Health Awards Benefiting Humanity Laureates". Tech Museum of Innovation. 2006. Retrieved 2009-01-07.
- ^ Lai CJ, Monath TP (2003). "Chimeric flaviviruses: novel vaccines against dengue fever, tick-borne encephalitis, and Japanese encephalitis". Advances in Virus Research. 61: 469–509. doi:10.1016/S0065-3527(03)61013-4. ISBN 9780120398614. PMID 14714441.
- ^ Querec T, Bennouna; Bennouna, S; Alkan, S; Laouar, Y; Gorden, K; Flavell, R; Akira, S; Ahmed, R; Pulendran, B (2006). "Yellow fever vaccine YF-17D activates multiple dendritic cell subsets via TLR2, 7, 8, and 9 to stimulate polyvalent immunity". J. Exp. Med. 203 (2): 413–24. doi:10.1084/jem.20051720. PMC 2118210. PMID 16461338.
- ^ Filomatori CV, Lodeiro MF, Alvarez DE, Samsa MM, Pietrasanta L, Gamarnik AV (2006). "A 5' RNA element promotes dengue virus RNA synthesis on a circular genome". Genes Dev. 20 (16): 2238–49. doi:10.1101/gad.1444206. PMC 1553207. PMID 16882970.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kinney RM, Huang CY, Rose BC; et al. (April 2005). "Inhibition of dengue virus serotypes 1 to 4 in vero cell cultures with morpholino oligomers". Journal of Virology. 79 (8): 5116–28. doi:10.1128/JVI.79.8.5116-5128.2005. PMC 1069583. PMID 15795296.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Burrer R, Neuman BW, Ting JP; et al. (June 2007). "Antiviral effects of antisense morpholino oligomers in murine coronavirus infection models". Journal of Virology. 81 (11): 5637–48. doi:10.1128/JVI.02360-06. PMC 1900280. PMID 17344287.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Stein DA, Huang CY, Silengo S; et al. (September 2008). "Treatment of AG129 mice with antisense morpholino oligomers increases survival time following challenge with dengue 2 virus". The Journal of Antimicrobial Chemotherapy. 62 (3): 555–65. doi:10.1093/jac/dkn221. PMC 7109848. PMID 18567576.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ "Project Summary". Discovering Dengue Drugs-Together. University of Texas, Medical Branch. 2007. Retrieved 2008-10-05.
- ^ Discovering Dengue Drugs-Together project status report
- ^ a b Fua, Guoliang; Leesa, Rosemary S.; Nimmoa, Derric; Awc, Diane; Jina, Li; Graya, Pam; Berendonkb, Thomas U.; White-Cooperb, Helen; Scaifea, Sarah (2010). "Female-specific flightless phenotype for mosquito control" (PDF). Proc. Natl. Acad. Sci. 107 (10): 4550–4554. doi:10.1073/pnas.1000251107. PMC 2826341. PMID 20176967..
- ^ 'Lame' mosquitoes to stop dengue. BBC News. 23 February 2010..
- ^ "Dengue & DHF: Information for Health Care Practitioners". Dengue Fever. CDC Division of Vector-Borne Infectious Diseases (DVBID). 2007-10-22. Retrieved 2008-10-05.
- ^ Takhampunya R, Ubol S, Houng HS, Cameron CE, Padmanabhan R (2006). "Inhibition of dengue virus replication by mycophenolic acid and ribavirin". J. Gen. Virol. 87 (Pt 7): 1947–52. doi:10.1099/vir.0.81655-0. PMID 16760396.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Brazil Scientists Discover "Cat's Claw" Combats Dengue Fever
- ^ Study on tawa-tawa as cure for dengue not yet done
- ^ Rothman AL (2004). "Dengue: defining protective versus pathologic immunity". J. Clin. Invest. 113 (7): 946–51. doi:10.1172/JCI200421512. PMC 379334. PMID 15057297.
- ^ Nowak MA, May RM (January 1994). "Superinfection and the evolution of parasite virulence". Proceedings. Biological Sciences / The Royal Society. 255 (1342): 81–9. doi:10.1098/rspb.1994.0012. PMID 8153140.
{{cite journal}}: CS1 maint: date and year (link) - ^ Levin SA, Pimentel D (1981). "Selection of intermediate rates of increase in parasite-host systems". American Naturalist. 117 (3): 308–15. doi:10.1086/283708.
- ^ Fernanda Pontes (20 March 2008). "Secretário estadual de Saúde Sérgio Côrtes admite que estado vive epidemia de dengue". O Globo Online (in Portuguese)..
- ^ CNN (3 April 2008). "Thousands hit by Brazil outbreak of dengue". CNN.
{{cite news}}:|author=has generic name (help). - ^ http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B7CPT-4KKNNH5-2&_user=130561&_rdoc=1&_fmt=&_orig=search&_sort=d&view=c&_acct=C000010878&_version=1&_urlVersion=0&_userid=130561&md5=4cc1b9743b4fddf5a0567b16b99bc130
- ^ Marcos Wozniak (12 March 2009).
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help). - ^ Sri Lanka
- ^ Wilder-Smith A, Chen LH, Massad E, Wilson ME (2009). "Threat of dengue to blood safety in dengue-endemic countries". Emerg Infect Dis. 15 (1): 8–11. doi:10.3201/eid1501.071097. PMC 2660677. PMID 19116042.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Stramer SL, Hollinger FB, Katz LM, Kleinman S, Metzel PS, Gregory KR, Dodd RY (2009). "Emerging infectious disease agents and their potential threat to transfusion safety". Transfusion. 49 (Suppl 2): 1–29. doi:10.1111/j.1537-2995.2008.02019.x. PMID 19686562.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Teo D, Ng LC, Lam S (2009). "Is dengue a threat to the blood supply?". Transfus Med. 19 (2): 66–77. doi:10.1111/j.1365-3148.2009.00916.x. PMC 2713854. PMID 19392949.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Dengue fever: essential data". 1999. Retrieved 2008-10-05.
- ^ Harper D (2001). "Etymology: dengue". Online Etymology Dictionary. Retrieved 2008-10-05.
- ^ a b "etymologia: dengue" (PDF). Emerging Infectious Diseases. 12 (6): 893. 2006. doi:10.3201/eid1206.ET1206.
- ^ url=http://www.medterms.com/script/main/art.asp?articlekey=6620
- ^ Gubler DJ (July 1998). "Dengue and dengue hemorrhagic fever". Clinical Microbiology Reviews. 11 (3): 480–96. doi:10.1128/CMR.11.3.480. PMC 88892. PMID 9665979.
{{cite journal}}: CS1 maint: date and year (link) - ^ Dengue Fever Fact Sheet. CDC.
- ^ "Chemical and Biological Weapons: Possession and Programs Past and Present", James Martin Center for Nonproliferation Studies, Middlebury College, April 9, 2002, accessed November 14, 2008.
- ^ "Discovering Dengue Drugs – Together". University of Texas Medical Branch. 2009-01-04. Retrieved 2009-01-04.
External links edit
- Dengue: CDC home page The Centers for Disease Control and Prevention (CDC)
- Dengue: Clinical and Public Health Aspects, The Centers for Disease Control and Prevention (CDC)
- Dengue haemorrhagic fever: diagnosis, treatment, prevention and control 2nd edition. Geneva : World Health Organization.
- The NCBI Virus Variation Resources The Virus Variation Resources at The National Center for Biotechnology Information (NCBI).
- Dengue Virus Net Information site for dengue symptoms, prevention, treatment, vaccine research and outbreak news.