Thiocolchicoside (Muscoril, Myoril, Neoflax) is a muscle relaxant with anti-inflammatory and analgesic effects.[3][4][5][6] Its mechanism of action is unknown, but it is believed to be act via antagonism of nicotinic acetylcholine receptors (nAchRs). However, it also appears to be a competitive antagonist of GABAA and glycine receptors.[7][8] As such, it has powerful convulsant activity and should not be used in seizure-prone individuals.[9][10][11]
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | Oral, Topical, IM |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 25%[1] |
| Elimination half-life | 5-6 hours[1][2] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.009.107 |
| Chemical and physical data | |
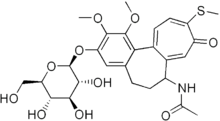
| Formula | C27H33NO10S |
| Molar mass | 563.62 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Medical uses
editLow back pain
editIn low back pain, thiocolchicoside is efficacious in reducing pain intensity, improving physical flexibility as seen in decreasing the distance from the hands to the floor when leaning forward without bending the knees (finger-floor distance), and reducing the total consumption of paracetamol.[12] Thiocolchicoside administration also leads to a reduction in muscle spasm during palpation, an improvement in the overall assessment of patients with low back pain, and an enhancement in their ability to perform daily activities.[12][13]
When thiocolchicoside is added to standard nonsteroidal anti-inflammatory drug (NSAID) therapy in lower back pain, such therapy reduces pain intensity and improves functional status according to the average estimates of visual analogue scale (VAS) and life disorders questionnaires. The use of thiocolchicoside in combination with NSAIDs results in a more pronounced decrease in pain when assessed by VAS, as well as an increase in functional activity based on an estimate of the distance from the fingertips to the floor by the 7th day of therapy (but not by the 3rd) compared with the use of NSAIDs alone.[12][13]
Several medicines, including tolperisone, aceclofenac plus tizanidine, and pregabalin, are effective in reducing pain intensity. Another comparative study found that eperisone with diclofenac was more effective in terms of finger-floor distance and improvement in Lasegue's sign (straight leg raise angle laying on back), VAS score, and global assessment scale than thiocolchicoside with diclofenac.[12][13][14]
Side effects
editSide effects of thiocolchicoside can include nausea, allergy and vasovagal reactions.[15] Liver injury, pancreatitis, seizures, blood cell disorders, severe cutaneous disorders, rhabdomyolysis, and reproductive disorders have all been recorded in the French and European pharmacovigilance databases and in the periodic updates that the companies concerned submit to regulatory agencies. These data do not specify the frequency of the disorders nor do they identify the most susceptible patient populations. Thiocolchicoside is teratogenic in experimental animals and also damages chromosomes. Human data are limited to a follow-up of about 30 pregnant women (no major malformations) and reports of altered spermatogenesis, including cases of azoospermia. In practice, there is no justification for exposing patients to the adverse effects of thiocolchicoside. It is better to use an effective, well-known analgesic for patients complaining of muscle pain, starting with paracetamol.[16]
Although muscle relaxants may have the major side effect of sedation, thiocolchicoside is free from sedation effects, likely due to its lack of potentiation of GABAA receptors.[7]
Pharmacokinetics
editThiocolchicoside is broken down in the body to a metabolite called 3-demethylthiocolchicine (also known as SL59.0955 or M2) that could damage dividing cells therefore inducing toxicity in the embryo, neoplastic changes and fertility reduction in males.[17] Therefore, recommended oral dose should not exceed 7 days and intramuscular dose duration should not exceed 5 days.[18] Local skin preparations are less toxic.[medical citation needed]
References
edit- ^ a b Perucca E, Poitou P, Pifferi G (1995). "Comparative pharmacokinetics and bioavailability of two oral formulations of thiocolchicoside, a GABA-mimetic muscle relaxant drug, in normal volunteers". European Journal of Drug Metabolism and Pharmacokinetics. 20 (4): 301–5. doi:10.1007/bf03190249. PMID 8983937. S2CID 13325496.
- ^ Sandouk P, Bouvier d'Yvoire M, Chretien P, Tillement JP, Scherrmann JM (January 1994). "Single-dose bioavailability of oral and intramuscular thiocolchicoside in healthy volunteers". Biopharmaceutics & Drug Disposition. 15 (1): 87–92. doi:10.1002/bdd.2510150108. PMID 8161719. S2CID 6712875.
- ^ Tüzün F, Unalan H, Oner N, Ozgüzel H, Kirazli Y, Içağasioğlu A, Kuran B, Tüzün S, Başar G (September 2003). "Multicenter, randomized, double-blinded, placebo-controlled trial of thiocolchicoside in acute low back pain". Joint, Bone, Spine. 70 (5): 356–61. doi:10.1016/S1297-319X(03)00075-7. PMID 14563464.
- ^ Ketenci A, Basat H, Esmaeilzadeh S (July 2009). "The efficacy of topical thiocolchicoside (Muscoril) in the treatment of acute cervical myofascial pain syndrome: a single-blind, randomized, prospective, phase IV clinical study". Agri. 21 (3): 95–103. PMID 19780000. Archived from the original on December 15, 2019. Retrieved April 8, 2010.
- ^ Soonawalla DF, Joshi N (May 2008). "Efficacy of thiocolchicoside in Indian patients suffering from low back pain associated with muscle spasm". Journal of the Indian Medical Association. 106 (5): 331–5. PMID 18839644.
- ^ Ketenci A, Ozcan E, Karamursel S (July 2005). "Assessment of efficacy and psychomotor performances of thiocolchicoside and tizanidine in patients with acute low back pain". International Journal of Clinical Practice. 59 (7): 764–70. doi:10.1111/j.1742-1241.2004.00454.x. PMID 15963201. S2CID 20671452.
- ^ a b Carta M, Murru L, Botta P, Talani G, Sechi G, De Riu P, Sanna E, Biggio G (September 2006). "The muscle relaxant thiocolchicoside is an agonist of GABAA receptor function in the central nervous system". Neuropharmacology. 51 (4): 805–15. doi:10.1016/j.neuropharm.2006.05.023. PMID 16806306. S2CID 11390033.
- ^ Mascia MP, Bachis E, Obili N, Maciocco E, Cocco GA, Sechi GP, Biggio G (March 2007). "Thiocolchicoside inhibits the activity of various subtypes of recombinant GABA(A) receptors expressed in Xenopus laevis oocytes". European Journal of Pharmacology. 558 (1–3): 37–42. doi:10.1016/j.ejphar.2006.11.076. PMID 17234181.
- ^ De Riu PL, Rosati G, Sotgiu S, Sechi G (August 2001). "Epileptic seizures after treatment with thiocolchicoside". Epilepsia. 42 (8): 1084–6. doi:10.1046/j.1528-1157.2001.0420081084.x. PMID 11554898. S2CID 24017279.
- ^ Giavina-Bianchi P, Giavina-Bianchi M, Tanno LK, Ensina LF, Motta AA, Kalil J (June 2009). "Epileptic seizure after treatment with thiocolchicoside". Therapeutics and Clinical Risk Management. 5 (3): 635–7. doi:10.2147/tcrm.s4823. PMC 2731019. PMID 19707540.
- ^ Sechi G, De Riu P, Mameli O, Deiana GA, Cocco GA, Rosati G (October 2003). "Focal and secondarily generalised convulsive status epilepticus induced by thiocolchicoside in the rat". Seizure. 12 (7): 508–15. doi:10.1016/S1059-1311(03)00053-0. PMID 12967581. S2CID 14308541.
- ^ a b c d Patel M, Shah R, Ramteke-Jadhav S, Patil V, Patel SK, Lila A, Shah N, Bandgar T (May 2020). "Систематический обзор по применению миорелаксантов при боли в нижней части спины" [Management of Insulin Autoimmune Hypoglycaemia: Single-centre experience from Western India with systematic review of world literature]. Clin Endocrinol (Oxf) (in Russian). 92 (5): 409–420. doi:10.1111/cen.14174. PMID 32064669.
- ^ a b c Petousis S, Margioula-Siarkou C, Kalogiannidis I (April 2016). "Effectiveness of Tocolytic Agents on Prevention of Preterm Delivery, Neonatal Morbidity, and Mortality: Is There a Consensus? A Review of the Literature". Obstet Gynecol Surv. 71 (4): 243–52. doi:10.1097/OGX.0000000000000302. PMID 27065070.
- ^ Qin Z, Zhang C, Guo J, Kwong JS, Li X, Pang R, Doiron RC, Nickel JC, Wu J (June 2022). "Oral pharmacological treatments for chronic prostatitis/chronic pelvic pain syndrome: A systematic review and network meta-analysis of randomised controlled trials". eClinicalMedicine. 48: 101457. doi:10.1016/j.eclinm.2022.101457. PMC 9125656. PMID 35706494.
- ^ Efe C, Purnak T, Ozaslan E, Milanlioglu A (March 2011). "Thiocolchicoside-induced liver injury". Clinics. 66 (3): 521–2. doi:10.1590/s1807-59322011000300029. PMC 3072020. PMID 21552685.
- ^ "Thiocolchicoside: review of adverse effects". Prescrire International. 25 (168): 41–3. February 2016. PMID 27042729.
- ^ "European Medicines Agency recommends restricting use of thiocolchicoside by mouth or injection". November 22, 2013. Archived from the original on April 21, 2024. Retrieved May 25, 2024.
- ^ "Thiocolchicoside-containing products for systemic use - important information regarding indications, treatment regimen, contraindications and warnings". February 7, 2024. Archived from the original on May 21, 2019.