Axial spondyloarthritis (also often referred to as axSpA) is a chronic, immune-mediated disease predominantly affecting the axial skeleton (sacroiliac joints and spine).[1] The term itself is an umbrella term characterizing a diverse disease family united by shared clinical and genetic features, such as the involvement of the axial skeleton.[2] The 2009 introduced term axial spondyloarthritis is a preferred term nowadays and substitutes the old term ankylosing spondylitis.[3]
| Axial spondyloarthritis | |
|---|---|
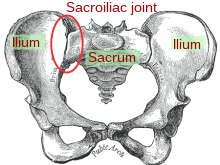 | |
| Sacroiliac joint |
Classification
editAlong with peripheral spondyloarthritis, reactive arthritis, psoriatic arthritis and enteropathic arthritis (or inflammatory bowel disease-associated spondyloarthritis), axial spondyloarthritis belongs to the spondyloarthritis disease family, also known as the spondyloarthritides or spondyloarthropathies.[4][5][6] These arthritic conditions can sometimes overlap with one another. For example, psoriatic arthritis can cause both peripheral and axial symptoms.[7] Likewise, reactive arthritis can transform into chronic axial spondyloarthritis.[8] All are considered inflammatory rheumatic disorders because they involve immune system-mediated attacks on the joints, muscles, bones and organs.[9]
Axial spondyloarthritis can be differentiated from peripheral spondyloarthritis in terms of the areas of the body affected. The axial form of the disease primarily affects the spine, pelvis and thoracic cage, whereas the peripheral form mainly targets the arms and legs.[10]
Axial spondyloarthritis can be divided into two classes:
- Non-radiographic axial spondyloarthritis (nr-axSpA):
This term encompasses both the early disease stage of ankylosing spondylitis, in which no radiographic changes are visible yet, as well as less severe forms of ankylosing spondylitis. - Radiographic axial spondyloarthritis:
Synonym for ankylosing spondylitis. This class is termed radiographic axial spondyloarthritis due to the unambiguous diagnosis through radiographic changes in the sacroiliac joints and/or spine.
Signs and symptoms
editAxial spondyloarthritis is predominantly marked by inflammatory pain and/or stiffness affecting the lower back, hips and/or buttocks.[11][12] The side affected may alternate.[11] Some may also experience symptoms in the eyes, rib cage, shoulders or cervical spine or neck as well.[12][13] Inflammatory back pain tends to come on gradually, become worse at night or after periods of rest (such as in the morning after waking up) and improve after exercise or the use of anti-inflammatory medications such as ibuprofen.[11][12] People with axial spondyloarthritis may experience alternating periods of remission and flare-ups.[14]
It is recommended that patients be formally evaluated for axial spondyloarthritis if they complain of inflammatory back pain and stiffness lasting at least three months, particularly if they are under the age of 45 and/or have a family history of the disease.[11]
Pathophysiology
editSignificant progress has been made in understanding the genetic and immunological aspects of axSpA. Research has focused on the mechanisms of chronic inflammation and pathological new bone formation, which are characteristic of the disease. The enthesis, a critical site of disease activity, is particularly affected. [15] The role of cytokine dysregulation in the immune pathogenesis of axSpA has been highlighted, with a notable skew towards a Th17 phenotype, tumor necrosis factor (TNF) and interleukin 23 (IL-23) / interleukin 17 (IL-17) pathways and a pro-inflammatory cytokine profile. The disease typically begins with enthesopathic inflammation and progresses to ossifying enthesitis. The molecular pathways involved in syndesmophyte formation are complex, involving factors such as bone morphogenetic protein, Wnt signaling pathway, Dickkopf-1, sclerostin, and various cytokines, all of which are intricately regulated. [16][17]
Diagnosis
editPatients being examined for axial spondyloarthritis may have x-rays, or radiographs, taken of their pelvis to check for signs of sacroilitis (often one of the first manifestations of the disease) and structural damage.[18] It can take several years from symptom onset for these changes to be visible, and some may never develop these changes at all.[19][20] Their presence distinguishes radiographic axial spondyloarthritis from nr-axSpA.
Patients may also undergo an MRI in place of or in addition to radiography. MRI technology is sensitive to inflammatory changes such as enthesitis and synovitis and is more specific overall.[19][21]
Blood work may also play a role in the diagnosis of axial spondyloarthritis. More than 80% of patients with the ankylosing spondylitis variant test positive for the HLA-B27 biomarker, but not everyone with this biomarker will develop disease.[22] Some people with axial spondyloarthritis may test positive for elevated C-reactive protein, or CRP, depending on their disease activity.[22] Spondyloarthritis is generally considered to be a seronegative disease, meaning tests for rheumatoid factor and other autoantibodies typically come back negative.[19][23]
Depending on the results of the above tests, patients may be referred to a rheumatologist for confirmation and follow-up.[24]
Prognosis
editSome with more severe disease may experience fusion of their vertebrae, a condition referred to as bamboo spine.[25] Men are more likely to accrue radiographic joint damage, whereas women tend to experience comparatively worse quality of life and disease activity.[26]
Management
editThere is currently no cure for axial spondyloarthritis, but there are various disease management strategies.[27]
Traditional NSAIDs and COX-2 inhibitor NSAIDs are effective for treating axSpA.[28] The potential harms may not differ when compared to a placebo treatment in the short term.[28] Various NSAIDs are equally effective (e.g.: Cox2 NSAIDS and traditional NSAIDS).[28] Continuous NSAID use may reduce radiographic spinal progression, but this requires confirmation.[28]
Those who cannot tolerate these medications or who require more intensive treatment may be prescribed biologic medications such as a TNF-alpha inhibitor in an attempt to alter the immune response driving the disease.[27]
Physical therapy and exercise have also been found to effectively address symptoms.[29]
In 2019 the American College of Rheumatology, Spondylitis Association of America and Spondyloarthritis Research and Treatment Network published updated recommendations for the treatment of the condition[30] based on updated literature reviews.
History
editIn 1984, a joint effort led to the definition of specific classification criteria for ankylosing spondylitis, called the "Modified New York criteria".[31] One of the central New York criteria was the existence of radiographically visible changes in the sacroiliac joints and/or spine, which have formed due to bone fusion, erosion and/or formation caused by the disease.[32] Even though these criteria helped to improve uniformly define ankylosing spondylitis, such radiologic changes often only manifested several years after the first disease symptoms appeared.[32] In order to be able to study also patients with early and less typical forms, new criteria were needed that could identify the disease already at an early stage. In 2009 the Modified New York criteria were extended by a broad set of new classification criteria that aimed to classify patients based on the presence of typical spondyloarthritis disease features.[2] These included inflammatory back pain, family history for axial spondyloarthritis, response to treatment with nonsteroidal anti-inflammatory drugs (NSAIDs), history of or current inflammation in the joints (arthritis), tendon-bone attachment of the heel (enthesitis), or eyes (uveitis), bowel (inflammatory bowel disease), skin (psoriasis) or signs of elevated inflammation (C-reactive protein and erythrocyte sedimentation rate).[2][33] Important parts of the ASAS axSpA criteria are the biomarker HLA-B27 and magnetic resonance imaging (MRI).[2][33] The criteria can only be applied in people that have chronic back pain (at least 3 months duration) started before the age of 45 years and only in those patients that already have a diagnosis of axial SpA. Since the disease ankylosing spondylitis was still defined by the Modified New York criteria of 1984, there was the need to find a new disease term that would also include the less severe forms or early onset of ankylosing spondylitis. This expression was found in the umbrella term axial spondyloarthritis. The 2009 classification criteria are called the ASAS (Assessment of SpondyloArthritis international Society) classification criteria for axial spondyloarthritis.[34][35]
Society and culture
editNotable cases
edit- Beau Biden[36]
- Talia Dean, The X-Factor[37]
- Zach Kornfeld, The Try Guys[38]
- Mick Mars, Mötley Crüe[39]
- Dan Reynolds, Imagine Dragons[40]
References
edit- ^ Sieper, Joachim; Poddubnyy, Denis (July 2017). "Axial spondyloarthritis". The Lancet. 390 (10089): 73–84. doi:10.1016/S0140-6736(16)31591-4. PMID 28110981.
- ^ a b c d Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J, et al. (June 2009). "The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection". Annals of the Rheumatic Diseases. 68 (6): 777–83. doi:10.1136/ard.2009.108233. PMID 19297344.
- ^ van der Heijde, Désirée; Molto, Anna; Ramiro, Sofia; Braun, Jürgen; Dougados, Maxime; van Gaalen, Floris A; Gensler, Lianne S; Inman, Robert D; Landewé, Robert B M; Marzo-Ortega, Helena; Navarro-Compán, Victoria; Phoka, Andri; Poddubnyy, Denis; Protopopov, Mikhail; Reveille, John (2023-12-08). "Goodbye to the term 'ankylosing spondylitis', hello 'axial spondyloarthritis': time to embrace the ASAS-defined nomenclature". Annals of the Rheumatic Diseases. 83 (5): ard–2023–225185. doi:10.1136/ard-2023-225185. hdl:1887/3764021. ISSN 0003-4967. PMID 38071514.
- ^ Kocatürk, Begüm; Balık, Zeynep; Pişiren, Gaye; Kalyoncu, Umut; Özmen, Füsun; Özen, Seza (2022). "Spondyloarthritides: Theories and beyond". Frontiers in Pediatrics. 10. doi:10.3389/fped.2022.1074239. ISSN 2296-2360. PMC 9816396. PMID 36619518.
- ^ "Spondyloarthritis". rheumatology.org. Retrieved 2023-04-23.
- ^ Zochling, J.; Brandt, J.; Braun, J. (2005-08-09). "The current concept of spondyloarthritis with special emphasis on undifferentiated spondyloarthritis". Rheumatology. 44 (12): 1483–1491. doi:10.1093/rheumatology/kei047. ISSN 1462-0332. PMID 16091395.
- ^ Schoels, M. M.; Braun, J.; Dougados, M.; Emery, P.; Fitzgerald, O.; Kavanaugh, A.; Kvien, T. K.; Landewé, R.; Luger, T.; Mease, P.; Olivieri, I.; Reveille, J.; Ritchlin, C.; Rudwaleit, M.; Sieper, J. (2014-01-01). "Treating axial and peripheral spondyloarthritis, including psoriatic arthritis, to target: results of a systematic literature search to support an international treat-to-target recommendation in spondyloarthritis". Annals of the Rheumatic Diseases. 73 (1): 238–242. doi:10.1136/annrheumdis-2013-203860. ISSN 0003-4967. PMC 3888585. PMID 23740234.
- ^ Inman, Robert D. (2021-04-01). "Axial Spondyloarthritis: Current Advances, Future Challenges". Journal of Rheumatic Diseases. 28 (2): 55–59. doi:10.4078/jrd.2021.28.2.55. PMC 10324891. PMID 37476012. S2CID 233561575.
- ^ Joseph, Amy; Brasington, Richard; Kahl, Leslie; Ranganathan, Prabha; Cheng, Tammy P.; Atkinson, John (2010-02-01). "Immunologic rheumatic disorders". Journal of Allergy and Clinical Immunology. 2010 Primer on Allergic and Immunologic Diseases. 125 (2, Supplement 2): S204–S215. doi:10.1016/j.jaci.2009.10.067. ISSN 0091-6749. PMID 20176259.
- ^ Taurog, Joel D.; Chhabra, Avneesh; Colbert, Robert A. (2016-06-30). Longo, Dan L. (ed.). "Ankylosing Spondylitis and Axial Spondyloarthritis". New England Journal of Medicine. 374 (26): 2563–2574. doi:10.1056/NEJMra1406182. ISSN 0028-4793. PMID 27355535.
- ^ a b c d Braun, Juergen; Inman, Robert (2010-07-01). "Clinical significance of inflammatory back pain for diagnosis and screening of patients with axial spondyloarthritis". Annals of the Rheumatic Diseases. 69 (7): 1264–1268. doi:10.1136/ard.2010.130559. ISSN 0003-4967. PMID 20566619. S2CID 12571711.
- ^ a b c Harper, Brock E.; Reveille, John D. (January 2009). "Spondyloarthritis: Clinical Suspicion, Diagnosis, and Sports". Current Sports Medicine Reports. 8 (1): 29–34. doi:10.1249/JSR.0b013e3181967ac6. ISSN 1537-8918. PMC 2898732. PMID 19142077.
- ^ Schwartzman, Sergio; Ruderman, Eric M. (2022-01-01). "A Road Map of the Axial Spondyloarthritis Continuum". Mayo Clinic Proceedings. 97 (1): 134–145. doi:10.1016/j.mayocp.2021.08.007. ISSN 0025-6196. PMID 34801248. S2CID 244422146.
- ^ Aouad, Krystel; Gossec, Laure (July 2022). "Defining and managing flares in axial spondyloarthritis". Current Opinion in Rheumatology. 34 (4): 195–202. doi:10.1097/BOR.0000000000000883. ISSN 1040-8711. PMID 35699318. S2CID 249645239.
- ^ McGonagle, Dennis; Aydin, Sibel Z.; Marzo-Ortega, Helena; Eder, Lihi; Ciurtin, Coziana (2021-12-01). "Hidden in plain sight: Is there a crucial role for enthesitis assessment in the treatment and monitoring of axial spondyloarthritis?". Seminars in Arthritis and Rheumatism. 51 (6): 1147–1161. doi:10.1016/j.semarthrit.2021.07.011. ISSN 0049-0172. PMID 34537464.
- ^ Ivanova, Mariana; Zimba, Olena; Dimitrov, Ivan; Angelov, Alexander K.; Georgiev, Tsvetoslav (2024-04-30). "Axial Spondyloarthritis: an overview of the disease". Rheumatology International. 44 (9): 1607–1619. doi:10.1007/s00296-024-05601-9. ISSN 1437-160X. PMID 38689098.
- ^ van de Sande, Marleen G.H.; Elewaut, Dirk (September 2023). "Pathophysiology and immunolgical basis of axial spondyloarthritis". Best Practice & Research Clinical Rheumatology. 37 (3): 101897. doi:10.1016/j.berh.2023.101897. PMID 38030467.
- ^ Navallas, María; Ares, Jesús; Beltrán, Brigitte; Lisbona, María Pilar; Maymó, Joan; Solano, Albert (June 2013). "Sacroiliitis Associated with Axial Spondyloarthropathy: New Concepts and Latest Trends". RadioGraphics. 33 (4): 933–956. doi:10.1148/rg.334125025. ISSN 0271-5333. PMID 23842966.
- ^ a b c Canella, Clarissa; Schau, Bruno; Ribeiro, Elisio; Sbaffi, Bruna; Marchiori, Edson (January 2013). "MRI in Seronegative Spondyloarthritis: Imaging Features and Differential Diagnosis in the Spine and Sacroiliac Joints". American Journal of Roentgenology. 200 (1): 149–157. doi:10.2214/AJR.12.8858. ISSN 0361-803X. PMID 23255756.
- ^ Rosenbaum, James T. (2016-07-03). "Evolving "Diagnostic" Criteria for Axial Spondyloarthritis in the Context of Anterior Uveitis". Ocular Immunology and Inflammation. 24 (4): 445–449. doi:10.3109/09273948.2016.1158277. ISSN 0927-3948. PMC 4993152. PMID 27070270.
- ^ Zochling, J.; Brandt, J.; Braun, J. (2005-12-01). "The current concept of spondyloarthritis with special emphasis on undifferentiated spondyloarthritis". Rheumatology. 44 (12): 1483–1491. doi:10.1093/rheumatology/kei047. ISSN 1462-0332. PMID 16091395.
- ^ a b Prajzlerová, Klára; Grobelná, Kristýna; Pavelka, Karel; Šenolt, Ladislav; Filková, Mária (2016-06-01). "An update on biomarkers in axial spondyloarthritis". Autoimmunity Reviews. 15 (6): 501–509. doi:10.1016/j.autrev.2016.02.002. ISSN 1568-9972. PMID 26851549.
- ^ Joseph, Amy; Brasington, Richard; Kahl, Leslie; Ranganathan, Prabha; Cheng, Tammy P.; Atkinson, John (2010-02-01). "Immunologic rheumatic disorders". Journal of Allergy and Clinical Immunology. 2010 Primer on Allergic and Immunologic Diseases. 125 (2, Supplement 2): S204–S215. doi:10.1016/j.jaci.2009.10.067. ISSN 0091-6749. PMID 20176259.
- ^ Poddubnyy, Denis; Tubergen, Astrid van; Landewé, Robert; Sieper, Joachim; Heijde, Désirée van der (2015-08-01). "Development of an ASAS-endorsed recommendation for the early referral of patients with a suspicion of axial spondyloarthritis". Annals of the Rheumatic Diseases. 74 (8): 1483–1487. doi:10.1136/annrheumdis-2014-207151. ISSN 0003-4967. PMID 25990288. S2CID 42585224.
- ^ Schwartzman, Sergio; Ruderman, Eric M. (2022-01-01). "A Road Map of the Axial Spondyloarthritis Continuum". Mayo Clinic Proceedings. 97 (1): 134–145. doi:10.1016/j.mayocp.2021.08.007. ISSN 0025-6196. PMID 34801248.
- ^ Rusman, T.; van Vollenhoven, R. F.; van der Horst-Bruinsma, I. E. (2018-05-12). "Gender Differences in Axial Spondyloarthritis: Women Are Not So Lucky". Current Rheumatology Reports. 20 (6): 35. doi:10.1007/s11926-018-0744-2. ISSN 1534-6307. PMC 5949138. PMID 29754330.
- ^ a b Lawson, Daeria O.; Eraso, Maria; Mbuagbaw, Lawrence; Joanes, Marianinha; Aves, Theresa; Leenus, Alvin; Omar, Ahmed; Inman, Robert D. (March 2020). "Tumor Necrosis Factor Inhibitor Dose Reduction for Axial Spondyloarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Arthritis Care & Research. 73 (6): 861–872. doi:10.1002/acr.24184. ISSN 2151-464X. PMID 32166872. S2CID 212692973.
- ^ a b c d Kroon FP, van der Burg LR, Ramiro S, Landewé RB, Buchbinder R, Falzon L, van der Heijde D (July 2015). "Non-steroidal anti-inflammatory drugs (NSAIDs) for axial spondyloarthritis (ankylosing spondylitis and non-radiographic axial spondyloarthritis)". The Cochrane Database of Systematic Reviews. 2015 (7): CD010952. doi:10.1002/14651858.CD010952.pub2. PMC 8942090. PMID 26186173.
- ^ Perrotta, Fabio Massimo; Musto, Antonio; Lubrano, Ennio (2019-12-01). "New Insights in Physical Therapy and Rehabilitation in Axial Spondyloarthritis: A Review". Rheumatology and Therapy. 6 (4): 479–486. doi:10.1007/s40744-019-00170-x. ISSN 2198-6584. PMC 6858478. PMID 31410786.
- ^ Ward MM, Deodhar A, Gensler LS, Dubreuil M, Yu D, Khan MA, et al. (October 2019). "2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis". Arthritis & Rheumatology. 71 (10): 1599–1613. doi:10.1002/art.41042. PMC 6764882. PMID 31436036.
- ^ van der Linden S, Valkenburg HA, Cats A (April 1984). "Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria". Arthritis and Rheumatism (Submitted manuscript). 27 (4): 361–8. doi:10.1002/art.1780270401. PMID 6231933.
- ^ a b Taurog JD, Chhabra A, Colbert RA (June 2016). "Ankylosing Spondylitis and Axial Spondyloarthritis". The New England Journal of Medicine. 374 (26): 2563–74. doi:10.1056/NEJMra1406182. PMID 27355535.
- ^ a b Poddubnyy D, van Tubergen A, Landewé R, Sieper J, van der Heijde D (August 2015). "Development of an ASAS-endorsed recommendation for the early referral of patients with a suspicion of axial spondyloarthritis". Annals of the Rheumatic Diseases. 74 (8): 1483–7. doi:10.1136/annrheumdis-2014-207151. PMID 25990288. S2CID 42585224.
- ^ Rudwaleit, M.; Landewé, R.; van der Heijde, D.; Listing, J.; Brandt, J.; Braun, J.; Burgos-Vargas, R.; Collantes-Estevez, E.; Davis, J.; Dijkmans, B.; Dougados, M.; Emery, P.; van der Horst-Bruinsma, I. E.; Inman, R.; Khan, M. A. (March 2009). "The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal". Annals of the Rheumatic Diseases. 68 (6): 770–776. doi:10.1136/ard.2009.108217. ISSN 1468-2060. PMID 19297345. S2CID 34185040.
- ^ Rudwaleit, M.; van der Heijde, D.; Landewé, R.; Listing, J.; Akkoc, N.; Brandt, J.; Braun, J.; Chou, C. T.; Collantes-Estevez, E.; Dougados, M.; Huang, F.; Gu, J.; Khan, M. A.; Kirazli, Y.; Maksymowych, W. P. (March 2009). "The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection". Annals of the Rheumatic Diseases. 68 (6): 777–783. doi:10.1136/ard.2009.108233. ISSN 1468-2060. PMID 19297344. S2CID 11515545.
- ^ House, The White (2021-05-28). "Remarks by President Biden Addressing Service Members and their Families". The White House. Retrieved 2023-04-22.
- ^ "Talia Dean: 'My back pain was misdiagnosed for 15 years - now I can't dance'". BBC News. 2021-01-15. Retrieved 2023-04-22.
- ^ Kornfeld, Zach. "I'm a founding member of 'The Try Guys' who launched a tea company that sold out in less than a day. Here's how I started and managed a successful business during the pandemic". Business Insider. Retrieved 2023-04-22.
- ^ Trepany, Charles. "Mötley Crüe guitarist Mick Mars retires due to health issues: 'The ultimate act of courage'". USA TODAY. Retrieved 2023-04-22.
- ^ "Imagine Dragons Lead Singer, Dan Reynolds, and CBS's "The Doctors" Raising Ankylosing Spondylitis Awareness!". Spondylitis Association of America - Ankylosing Spondylitis. Retrieved 2023-04-22.