Prostaglandin E2 receptor 4 (EP4) is a prostaglandin receptor for prostaglandin E2 (PGE2) encoded by the PTGER4 gene in humans;[5] it is one of four identified EP receptors, the others being EP1, EP2, and EP3, all of which bind with and mediate cellular responses to PGE2 and also, but generally with lesser affinity and responsiveness, certain other prostanoids (see Prostaglandin receptors). EP4 has been implicated in various physiological and pathological responses in animal models and humans.[6]
Gene
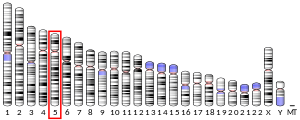
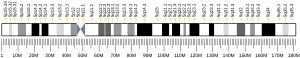
editThe PTGER4 gene is located on human chromosome 5p13.1 at position p13.1 (i.e. 5p13.1), contains 7 exons, and codes for a G protein-coupled receptor (GPCR) of the rhodopsin-like receptor family, Subfamily A14 (see rhodopsin-like receptors#Subfamily A14).[7] [8]
Expression
editIn humans, mRNA for EP4 has been detected by northern blotting in the heart and small intestine and to lesser extents in lung, kidney, thymus, uterus, dorsal root ganglions, and brain. EP4 protein is found in humans as measured by immunochemistry in pulmonary veins; kidney glomeruli and tunica media of kidney arteries; corpus cavernosum of the penis; carotid artery atherosclerotic plaques; Abdominal aorta aneurysms; corneal endothelium, corneal keratocytes, trabecular cells, ciliary epithelium, conjunctival stromal cells, and iridal stromal cells of the eye; and gingival fibroblasts.[9][10][11]
Ligands
editActivating ligands
editStandard prostanoids have the following relative efficacies in binding to and activating EP4: PGE2>PGF2α=PGI2>PGD2=TXA2. Prostaglandin E1 (PGE1), which has one less double bond than PGE2, has the same binding affinity and potency for EP4, both PGs having high affinity (Ki=3 nM) (http://www.guidetopharmacology.org/GRAC/ObjectDisplayForward?objectId=343).[12] Several synthetic compounds, e.g. 1-hydroxy-PGE1, rivenprost (ONO-4819), OOG-308, ONO-AE1-329, AGN205203, ONO-4819, CP-734,432m AE1-329, SC-19220, SC-51089, and EP4RAG bind to and stimulate EP4 but unlike PGE2 have the advantage of being selective for this receptor over other EP receptors and are relatively resistant to being metabolically degraded. They are in development as drugs for the potential treatment of various diseases including ulcerative colitis, Alzheimer's disease, osteoporosis, and certain cardiovascular diseases.[13]
Inhibiting ligands
editInhibitory receptor antagonists for EP4, including grapiprant (CJ-023,423), ONO-AE3-208, GW627368X, AH23848, and ONO-AE2-227, are in development for possible clinical use as inhibitors of the progression of prostate, breast, colon, and lung cancers.[13]
Mechanism of cell activation
editEP4 is classified as a relaxant type of prostaglandin receptor based on its ability, upon activation, to relax the contraction of certain smooth muscle preparations and smooth muscle-containing tissues that have been pre-contracted by stimulation.[6] When bound to PGE2 or other of its agonists, it mobilizes G proteins containing the Gs alpha subunit (i.e. Gαs)-G beta-gammaes (i.e. Gβγ) complex. The complex then dissociate into its Gαs and Gβγ components which act to regulate cell signaling pathways. In particular, Gαs stimulates adenyl cyclase to raise cellular levels of cAMP; cAMP activates PKA, a kinase which in turn activates signaling molecules, in particular, the transcription factor, CREB. Activated CREB stimulates the expression of genes such as c-fos, somatostatin, and corticotropin-releasing hormone that regulate cellular proliferation, cellular differentiation, cellular survival, and angiogenesis. EP4 activation of G proteins also activate PI3K/AKT/mTOR, ERK, and p38 MAPK pathways. Activation of ERK induces expression of EGR1, a transcription factor which controls transcription of genes involved in cellular differentiation and mitogenesis. EP4 also interacts with Prostaglandin E receptor 4-associated protein (EPRAP) to inhibit phosphorylation of the proteasome protein, p105, thereby suppressing a cells ability to activate nuclear factor kappa B, a transcription factor that controls genes coding for cytokines and other elements that regulate inflammation, cell growth, and cell survival (see NF-κB#Structure). The activation of these pathways lead to variety of different types of functional responses depending on cell type, the pathways available in different cell types, and numerous other factors; EP4 activation may therefore have diverse effects on cell function depending on these factors.[6][14] In many respects, EP4 actions resemble those of another type of another relaxant prostanoid receptor, EP2 but differs from the contractile prostanoid receptors, EP1 and EP3 receptors which mobilize G proteins containing the Gαq-Gβγ complex.[15][16]
Following its activation, EP4 undergoes homologous desensitization. That is, EP4 becomes insensitive to further activation and internalizes. This effect limits the duration and extent to which EP4 can stimulate cells. Agents which activate certain isoforms of protein kinase C can also desensitize EP4 by a process termed heterologous desensitization.[16]
Functions
editStudies using animals genetically engineered to lack EP4 and supplemented by studies examining the actions of EP4 receptor antagonists and agonists in animals as well as animal and human tissues indicate that this receptor serves various functions. However, an EP4 receptor function found in these studies does not necessarily indicate that in does so in humans since EP receptor functions can vary between species.[14]
Ductus arteriosus
editEP4 plays a critical role in postnatal closure of the ductus arteriosus as defined in mice lacking a functional gene for this receptor, i.e. EP4(-/-) mice (see Knockout mouse). About 95% of EP4(-/-) mice die within 3 days of birth due to the pulmonary congestion and heart failure caused by a patent ductus arteriosus. The ductus operates in the fetus to shunt blood from the pulmonary artery to the proximal descending aorta thereby allowing blood from the heart's right ventricle to bypass the fetus's non-functioning lungs. The ductus must close at birth to allow blood flow into the lungs. In mice, this is accomplished by turning off the mechanism which maintains the ductus's patency. Continuous activation of EP4 by PGE2 keeps the ductus open in the fetus; at birth, however, levels of EP4 and PGE2 in the smooth muscle cells and media in mouse ductus fall. This closes the ductus thereby establishing normal post-fetal circulation of blood through the lungs. Based on studies using EP receptor agonists and receptor antagonists, EP2 in mice and, at least in lambs, EP3 may play minor parts in maintaining patency of the ductus.[6][17][18] These studies also appear relevant to humans: nonsteroidal anti-inflammatory drugs, particularly indomethacin, are used to reduce prostaglandin production and thereby close the ductus in neonates, infants, and older patients with Patent ductus arteriosus; furthermore, prostaglandins or their analogs are used to keep the ductus open in neonates with congenital heart defects such as Transposition of the great arteries until corrective surgery can be performed (see Ductus arteriosus#Disorder: Patent ductus arteriosus).[6]
To allow further studies of EP4 function, colonies obtained by cross-breeding the 5% of mice surviving EP4 deletion are used.[6]
Inflammation
editActivation of EP4 suppresses the production of IL-12p70 and increases IL-23 thereby promoting development of IL-17-producing Th17 cells, a subset of pro-inflammatory T helper cells that serves to maintain mucosal barriers, clear mucosal surfaces of pathogens, and contribute to autoimmune and inflammatory disorders. Its activation also: a) supports the development of Regulatory T cells (i.e. suppressor T cells that modulate the immune system to maintain tolerance to self-antigens and prevent autoimmune disease); b) stimulate Dendritic cells (i.e. antigen-presenting cells located primarily in the skin and mucous membranes) to mature, migrate, and direct the early stage of immune responses; c) inhibit antibody-producing B cells from proliferating; d) suppresses the development of Atherosclerosis plaques by promoting the death (i.e. apoptosis) of plaque-bound pro-inflammatory macrophages; e) increases the survival of neurons in an inflammation-based model of Alzheimer's disease; f) increases local arteriole and capillary blood flow to cause, for example, site-specific signs of inflammation such as redness, heat, and swelling in rodent models; and g) suppresses sensory Dorsal root ganglion neurons from signaling inflammation-induced pain (i.e. allodynia and hyperalgesia) and has been used successfully to block the osteoarthritis pain in dogs.[6][15][19][13]
EP4 receptors are highly expressed in the small intestine and colon. Mice lacking this receptor or treated with a selective EP4 antagonist proved to be far more susceptible to the development of dextran sodium sulphate (DSS)-induced colitis and to be protected from developing the colitis by pre-treatment with EP4-selective agonists (ONO-AE1-734 and AGN205203). The DDS-inflicted lesions were associated with defective colon mucosa barrier function along with the overexpression of genes mediating inflammatory responses and under-expression of genes involved in mucosal repair and remodeling. EP4 thus appears to serve anti-inflammatory and protective functions in the colon and agonists of this receptor may be useful for treating inflammatory bowel diseases such as ulcerative colitis.[19] Activation of EP4 stimulates duodenum epithelial cells to secrete bicarbonate (HCO3-) in mice and humans; this response neutralizes the acidic fluid flowing from the stomach thereby contributing to the process of intestinal ulcer healing. Activators of this receptor therefore may useful as anti-ulcer drugs.[14]
Bone
editStudies in mice found that the PGE2-EP4 pathway induces osteoclast (i.e. cells responsible for bone absorption) to differentiate from precursor cells and is required for IL-1beta-, Tumor necrosis factor alpha-, and basic fibroblast growth factor-induced osteoclast formation; bone taken from EP4(-/-) mice to re-absorb bone when induced to do so and the infusion of PGE2 into mice failed to stimulate bone absorption. Furthermore, the infusion of selective EP4 agonists into mice stimulated increases in the number of bone osteoclasts and osteoblasts as well as increases in bone density. These studies indicate that the EP4 receptor mediates bone remolding in mice and, it is suggested, other animals including humans.[6]
Heart
editIn mice, EP4 receptor agonists reduce the acute rejection of transplanted hearts, prolong the survival of heart-transplanted animals, and reduce cardiac damage in a model of ischemic reperfusion injury but also stimulate cardiac hypertrophy accompanied by poor cardiac function. EP4 receptor-depleted mice exhibit more severe cardiac damage in experimental models of myocardial infarction and ischemic reperfusion injury but also develop cardiac hypertrophy with poor cardiac function.[11] Cardiac specific EP4 deficiency using Site-specific recombination by the Cre recombinase method to inactivate EP4 only in cardiac muscle causes a somewhat different form of cardiac disease, dilated cardiomyopathy, that develops within 23–33 weeks after birth in mice.[6] These studies are interpreted as indicating that EP4 plays both protective and damaging roles in the heart with the protective effects of EP4 due at least in part to its ability to suppress inflammation.
Lipid metabolism
editEP4 receptor-depleted mice exhibit slower weight gain; reduced adiposity upon high fat diet challenge; and shortened life span. These deficiencies are associated with disrupted lipid metabolism due to impaired triglyceride clearance; this impaired triglyceride clearance may underlie the cited deficiencies.[11][20]
Cancer
editThe EP4 receptor is over-expressed in human prostate cancer tissue and a selective EP4-receptor antagonist inhibits the growth and metastasis of human prostate cancer cell xenografts. An EP4 receptor antagonist as well EP4 Gene knockdown inhibit the in vitro proliferation and invasiveness of human breast cancer cells. And, gene knockdown of EP4 inhibit the metastasis of murine breast cancer cells in a mouse model of induced breast cancer. PGE2 stimulates the in vitro growth of human non-small cell lung cancer while an antagonist of EP4 or EP4 gene knockdown inhibits this growth. These results indicate that the stimulation of EP4 promotes the growth of various types of cancer cells and therefore may play a role in the progression of certain types of human cancer.[13]
Hearing
editEP44 receptors are expressed in the cochlea of the inner ear. Pre- and post-treatment of guinea pigs with an EP4 agonist significantly attenuated threshold shifts of auditory brain stem responses and significantly reduced the loss of outer hair cells caused by prior noise exposure. These findings indicate that EP4 is involved in mechanisms for prostaglandin E(1) actions on the cochlea, and local EP4 agonist treatment may be a means for attenuating noise-induced hearing lose.[21][6]
Eye
editA selective EP4 antagonists significantly reduced corneal neovascularization in rats caused by oxygen-induced retinopathy or laser-induced choroidal neovascularization. This result suggests that EP4 activation contributes to corneal neovascularization and that EP4 antagonists may be useful for treating neovascular eye disease.[6]
Clinical significance
editTranslational research
editClinical translational research studies using EP4 stimulators (i.e. agonists) or inhibitors (i.e. antagonists) that have been conducted or are underway include:
- The selective EP4 agonist, name
rivenprost (ONO-4819), improved the ulcerative colitis symptoms of 3 among 4 tested patients in a phase 2 clinical trial finished in 2009 (https://clinicaltrials.gov/ct2/show/record/NCT00296556?term=rivenprost&rank=10) but no follow-up studies have been recorded.[13] - The EP4 selective antagonist, CJ-023,423, was tested for its effectiveness in treating gastroduodenal ulcers in patients between 2006 and 2008 d with no results reported (https://clinicaltrials.gov/ct2/show/NCT00392080?term=CJ-023%2C423&rank=1) and is currently being tested in the recruitment step for a phase 2 clinical trial to treat prostate, non-small cell lung, and breast cancers (https://clinicaltrials.gov/ct2/show/NCT02538432?term=CJ-023%2C423&rank=2).[13]
- The EP4 selective antagonist, BGC20-1531, is being tested for its ability to block PGE2-induced headaches in health volunteers to determine if it is a potentially useful candidate for testing its effectiveness on clinical headaches (https://clinicaltrials.gov/ct2/show/NCT00957983?term=EP4&rank=1).
- Grapiprant, a highly selective and potent EP4 antagonist, is approved by the Food and Drug Administration for use in canine medicine to treat pain caused by inflammation such as that occurring in osteoarthritis;[22] it is currently also under investigation for use in humans.[23]
Genomic Studies
editSingle nucleotide polymorphism (SNP) A/G variant rs10440635[24] close to the PTGER4 gene on human chromosome 5 has been associated with an increased incidence of Ankylosing spondylitis in a population recruited from the United Kingdom, Australia, and Canada. Ankylosing spondylitis is a chronic inflammatory disease involving excessive bone deposition in the Vertebral column and increased expression of EP4 at vertebral column sites of involvement. Thus, excessive EP4 activation may contribute to the pathological bone remodeling and deposition found in ankylosing spondylitis and the rs10440635 variant may predispose to this disease by influencing EP4's production or expression pattern.[25][26]
The GG genotype at -1254G>A in PTGER4 is associated with the non-steroidal anti-inflammatory drug (NSAID)-exacerbated cutaneous disease (NECD). NECD is a non-allergic hypersensitivity reaction involving the acute development of wheals and angioedema in response to NSAID consumption in individuals with a history of chronic urticarial. The G allele at the -1254 position leads to lower PTGER4 gene promoter function, lower levels of EP4, and presumably thereby less of the anti-inflammatory effects of EP4.[27]
Several PTGER4 gene variations have been associated with inflammatory bowel disease: a) Meta-analysis of Genome-wide association studies found that SNP variant rs11742570[28] containing a C/T single-nucleotide variation in PTGER4 is associated with an increased incidence of Crohn's disease; b) rs4495224,[29] an A/C SNP variant, and rs7720838,[30] both of which are projected to be binding sites in PTERG4 for the transcription factor, NF-κB, have been associated with Crohn's disease in three independent cohorts with the association between rs7720838 and Crohn's disease being replicated in other populations; and c) certain alleles in 5p13.1, a Gene desert close to PTGER4, correlate with the expression levels of EP4 as well as with the development of Crohn's disease.[27]
The A/T SNP variant, rs4434423,[31] in the 5'-untranslated region of PTGER4 has been associated with and increase rate of primary graft dysfunction in a multicentered cohort study of graph recipients of different ethnicities.[27]
See also
editReferences
edit- ^ a b c GRCh38: Ensembl release 89: ENSG00000171522 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000039942 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "PTGER3 prostaglandin e receptor 3 [Homo sapiens (Human)] - Gene - NCBI". Archived from the original on 2016-02-26. Retrieved 2017-01-24.
- ^ a b c d e f g h i j k Woodward DF, Jones RL, Narumiya S (September 2011). "International Union of Basic and Clinical Pharmacology. LXXXIII: classification of prostanoid receptors, updating 15 years of progress". Pharmacological Reviews. 63 (3): 471–538. doi:10.1124/pr.110.003517. PMID 21752876.
- ^ "PTGER4 prostaglandin e receptor 4 [Homo sapiens (Human)] - Gene - NCBI". Archived from the original on 2017-02-11. Retrieved 2017-02-06.
- ^ "Entrez Gene: PTGER4 prostaglandin E receptor 4 (subtype EP4)". Archived from the original on 2010-12-05.
- ^ "EP4 receptor - Prostanoid receptors - IUPHAR/BPS Guide to PHARMACOLOGY". www.guidetopharmacology.org. Archived from the original on 2 January 2018. Retrieved 6 May 2018.
- ^ Ichikawa A, Sugimoto Y, Tanaka S (2010). "Molecular biology of histidine decarboxylase and prostaglandin receptors". Proceedings of the Japan Academy. Series B, Physical and Biological Sciences. 86 (8): 848–66. Bibcode:2010PJAB...86..848I. doi:10.2183/pjab.86.848. PMC 3037517. PMID 20948178.
- ^ a b c Pang L, Cai Y, Tang EH, Irwin MG, Ma H, Xia Z (2016). "Prostaglandin E Receptor Subtype 4 Signaling in the Heart: Role in Ischemia/Reperfusion Injury and Cardiac Hypertrophy". Journal of Diabetes Research. 2016: 1324347. doi:10.1155/2016/1324347. PMC 4846751. PMID 27190998.
- ^ Narumiya S, Sugimoto Y, Ushikubi F (October 1999). "Prostanoid receptors: structures, properties, and functions". Physiological Reviews. 79 (4): 1193–226. doi:10.1152/physrev.1999.79.4.1193. PMID 10508233. S2CID 7766467.
- ^ a b c d e f Markovič T, Jakopin Ž, Dolenc MS, Mlinarič-Raščan I (January 2017). "Structural features of subtype-selective EP receptor modulators". Drug Discovery Today. 22 (1): 57–71. doi:10.1016/j.drudis.2016.08.003. PMID 27506873.
- ^ a b c Moreno JJ (February 2017). "Eicosanoid receptors: Targets for the treatment of disrupted intestinal epithelial homeostasis". European Journal of Pharmacology. 796: 7–19. doi:10.1016/j.ejphar.2016.12.004. PMID 27940058. S2CID 1513449.
- ^ a b Kalinski P (January 2012). "Regulation of immune responses by prostaglandin E2". Journal of Immunology. 188 (1): 21–8. doi:10.4049/jimmunol.1101029. PMC 3249979. PMID 22187483.
- ^ a b Korbecki J, Baranowska-Bosiacka I, Gutowska I, Chlubek D (2014). "Cyclooxygenase pathways". Acta Biochimica Polonica. 61 (4): 639–49. doi:10.18388/abp.2014_1825. PMID 25343148.
- ^ Ushikubi F, Sugimoto Y, Ichikawa A, Narumiya S (August 2000). "Roles of prostanoids revealed from studies using mice lacking specific prostanoid receptors". Japanese Journal of Pharmacology. 83 (4): 279–85. doi:10.1254/jjp.83.279. PMID 11001172.
- ^ Bouayad A, Kajino H, Waleh N, Fouron JC, Andelfinger G, Varma DR, Skoll A, Vazquez A, Gobeil F, Clyman RI, Chemtob S (May 2001). "Characterization of PGE2 receptors in fetal and newborn lamb ductus arteriosus". American Journal of Physiology. Heart and Circulatory Physiology. 280 (5): H2342-9. doi:10.1152/ajpheart.2001.280.5.H2342. PMID 11299240. S2CID 32049750.
- ^ a b Hohjoh H, Inazumi T, Tsuchiya S, Sugimoto Y (December 2014). "Prostanoid receptors and acute inflammation in skin". Biochimie. 107 Pt A: 78–81. doi:10.1016/j.biochi.2014.08.010. PMID 25179301.
- ^ Cai Y, Ying F, Song E, Wang Y, Xu A, Vanhoutte PM, Tang EH (December 2015). "Mice lacking prostaglandin E receptor subtype 4 manifest disrupted lipid metabolism attributable to impaired triglyceride clearance". FASEB Journal. 29 (12): 4924–36. doi:10.1096/fj.15-274597. PMID 26271253. S2CID 28363263.
- ^ Hori R, Nakagawa T, Sugimoto Y, Sakamoto T, Yamamoto N, Hamaguchi K, Ito J (June 2009). "Prostaglandin E receptor subtype EP4 agonist protects cochleae against noise-induced trauma". Neuroscience. 160 (4): 813–9. doi:10.1016/j.neuroscience.2009.03.014. hdl:2433/120543. PMID 19303430. S2CID 23372528.
- ^ De Vito V, Salvadori M, Poapolathep A, Owen H, Rychshanova R, Giorgi M (October 2017). "Pharmacokinetic/pharmacodynamic evaluation of grapiprant in a carrageenan-induced inflammatory pain model in the rabbit". Journal of Veterinary Pharmacology and Therapeutics. 40 (5): 468–475. doi:10.1111/jvp.12380. PMID 27925221. S2CID 4170611.
- ^ Okumura Y, Yamagishi T, Nukui S, Nakao K (March 2017). "Discovery of AAT-008, a novel, potent, and selective prostaglandin EP4 receptor antagonist". Bioorganic & Medicinal Chemistry Letters. 27 (5): 1186–1192. doi:10.1016/j.bmcl.2017.01.067. PMID 28169162.
- ^ snpdev. "Reference SNP (refSNP) Cluster Report: rs10440635". www.ncbi.nlm.nih.gov. Archived from the original on 18 February 2017. Retrieved 6 May 2018.
- ^ Evans DM, Spencer CC, Pointon JJ, Su Z, Harvey D, Kochan G, Oppermann U, Opperman U, Dilthey A, Pirinen M, Stone MA, Appleton L, Moutsianas L, Moutsianis L, Leslie S, Wordsworth T, Kenna TJ, Karaderi T, Thomas GP, Ward MM, Weisman MH, Farrar C, Bradbury LA, Danoy P, Inman RD, Maksymowych W, Gladman D, Rahman P, Morgan A, Marzo-Ortega H, Bowness P, Gaffney K, Gaston JS, Smith M, Bruges-Armas J, Couto AR, Sorrentino R, Paladini F, Ferreira MA, Xu H, Liu Y, Jiang L, Lopez-Larrea C, Díaz-Peña R, López-Vázquez A, Zayats T, Band G, Bellenguez C, Blackburn H, Blackwell JM, Bramon E, Bumpstead SJ, Casas JP, Corvin A, Craddock N, Deloukas P, Dronov S, Duncanson A, Edkins S, Freeman C, Gillman M, Gray E, Gwilliam R, Hammond N, Hunt SE, Jankowski J, Jayakumar A, Langford C, Liddle J, Markus HS, Mathew CG, McCann OT, McCarthy MI, Palmer CN, Peltonen L, Plomin R, Potter SC, Rautanen A, Ravindrarajah R, Ricketts M, Samani N, Sawcer SJ, Strange A, Trembath RC, Viswanathan AC, Waller M, Weston P, Whittaker P, Widaa S, Wood NW, McVean G, Reveille JD, Wordsworth BP, Brown MA, Donnelly P (July 2011). "Interaction between ERAP1 and HLA-B27 in ankylosing spondylitis implicates peptide handling in the mechanism for HLA-B27 in disease susceptibility". Nature Genetics. 43 (8): 761–7. doi:10.1038/ng.873. PMC 3640413. PMID 21743469.
- ^ Haroon N (June 2015). "Ankylosis in ankylosing spondylitis: current concepts". Clinical Rheumatology. 34 (6): 1003–7. doi:10.1007/s10067-015-2956-4. PMID 25935456. S2CID 25930196.
- ^ a b c Cornejo-García JA, Perkins JR, Jurado-Escobar R, García-Martín E, Agúndez JA, Viguera E, Pérez-Sánchez N, Blanca-López N (2016). "Pharmacogenomics of Prostaglandin and Leukotriene Receptors". Frontiers in Pharmacology. 7: 316. doi:10.3389/fphar.2016.00316. PMC 5030812. PMID 27708579.
- ^ "No items found - Gene - NCBI". www.ncbi.nlm.nih.gov. Archived from the original on 19 February 2017. Retrieved 6 May 2018.
- ^ "No items found - Gene - NCBI". www.ncbi.nlm.nih.gov. Archived from the original on 4 March 2017. Retrieved 6 May 2018.
- ^ "PTGER4 prostaglandin e receptor 4 [Homo sapiens (Human)] - Gene - NCBI". Archived from the original on 2018-05-06. Retrieved 2017-02-19.
- ^ "No items found - Gene - NCBI". www.ncbi.nlm.nih.gov. Archived from the original on 4 March 2017. Retrieved 6 May 2018.
External links
edit- "Prostanoid Receptors: EP4". IUPHAR Database of Receptors and Ion Channels. International Union of Basic and Clinical Pharmacology. Archived from the original on 2016-03-03. Retrieved 2008-12-09.
Further reading
edit- Duncan AM, Anderson LL, Funk CD, Abramovitz M, Adam M (February 1995). "Chromosomal localization of the human prostanoid receptor gene family". Genomics. 25 (3): 740–2. doi:10.1016/0888-7543(95)80022-E. PMID 7759114.
- Wu H, Wu T, Hua W, Dong X, Gao Y, Zhao X, Chen W, Cao W, Yang Q, Qi J, Zhou J, Wang J (March 2015). "PGE2 receptor agonist misoprostol protects brain against intracerebral hemorrhage in mice". Neurobiology of Aging. 36 (3): 1439–50. doi:10.1016/j.neurobiolaging.2014.12.029. PMC 4417504. PMID 25623334.
- Regan JW, Bailey TJ, Pepperl DJ, Pierce KL, Bogardus AM, Donello JE, Fairbairn CE, Kedzie KM, Woodward DF, Gil DW (August 1994). "Cloning of a novel human prostaglandin receptor with characteristics of the pharmacologically defined EP2 subtype". Molecular Pharmacology. 46 (2): 213–20. PMID 8078484.
- Bastien L, Sawyer N, Grygorczyk R, Metters KM, Adam M (April 1994). "Cloning, functional expression, and characterization of the human prostaglandin E2 receptor EP2 subtype". The Journal of Biological Chemistry. 269 (16): 11873–7. doi:10.1016/S0021-9258(17)32654-6. PMID 8163486.
- An S, Yang J, Xia M, Goetzl EJ (November 1993). "Cloning and expression of the EP2 subtype of human receptors for prostaglandin E2". Biochemical and Biophysical Research Communications. 197 (1): 263–70. doi:10.1006/bbrc.1993.2470. PMID 8250933.
- Foord SM, Marks B, Stolz M, Bufflier E, Fraser NJ, Lee MG (July 1996). "The structure of the prostaglandin EP4 receptor gene and related pseudogenes". Genomics. 35 (1): 182–8. doi:10.1006/geno.1996.0337. PMID 8661119.
- Fedyk ER, Phipps RP (October 1996). "Prostaglandin E2 receptors of the EP2 and EP4 subtypes regulate activation and differentiation of mouse B lymphocytes to IgE-secreting cells". Proceedings of the National Academy of Sciences of the United States of America. 93 (20): 10978–83. Bibcode:1996PNAS...9310978F. doi:10.1073/pnas.93.20.10978. PMC 38269. PMID 8855294.
- Mori K, Tanaka I, Kotani M, Miyaoka F, Sando T, Muro S, Sasaki Y, Nakagawa O, Ogawa Y, Usui T, Ozaki S, Ichikawa A, Narumiya S, Nakao K (June 1996). "Gene expression of the human prostaglandin E receptor EP4 subtype: differential regulation in monocytoid and lymphoid lineage cells by phorbol ester". Journal of Molecular Medicine. 74 (6): 333–6. doi:10.1007/BF00207510. hdl:2433/160737. PMID 8862514. S2CID 20377539.
- Mukhopadhyay P, Geoghegan TE, Patil RV, Bhattacherjee P, Paterson CA (May 1997). "Detection of EP2, EP4, and FP receptors in human ciliary epithelial and ciliary muscle cells". Biochemical Pharmacology. 53 (9): 1249–55. doi:10.1016/S0006-2952(97)00011-7. PMID 9214685.
- Cosme R, Lublin D, Takafuji V, Lynch K, Roche JK (July 2000). "Prostanoids in human colonic mucosa: effects of inflammation on PGE(2) receptor expression". Human Immunology. 61 (7): 684–96. doi:10.1016/S0198-8859(00)00131-2. PMID 10880739.
- Desai S, April H, Nwaneshiudu C, Ashby B (December 2000). "Comparison of agonist-induced internalization of the human EP2 and EP4 prostaglandin receptors: role of the carboxyl terminus in EP4 receptor sequestration". Molecular Pharmacology. 58 (6): 1279–86. doi:10.1124/mol.58.6.1279. PMID 11093764.
- Sales KJ, Katz AA, Davis M, Hinz S, Soeters RP, Hofmeyr MD, Millar RP, Jabbour HN (May 2001). "Cyclooxygenase-2 expression and prostaglandin E(2) synthesis are up-regulated in carcinomas of the cervix: a possible autocrine/paracrine regulation of neoplastic cell function via EP2/EP4 receptors". The Journal of Clinical Endocrinology and Metabolism. 86 (5): 2243–9. doi:10.1210/jcem.86.5.7442. PMC 2694306. PMID 11344234.
- Faour WH, He Y, He QW, de Ladurantaye M, Quintero M, Mancini A, Di Battista JA (August 2001). "Prostaglandin E(2) regulates the level and stability of cyclooxygenase-2 mRNA through activation of p38 mitogen-activated protein kinase in interleukin-1 beta-treated human synovial fibroblasts". The Journal of Biological Chemistry. 276 (34): 31720–31. doi:10.1074/jbc.M104036200. PMID 11423555.
- Desai S, Ashby B (July 2001). "Agonist-induced internalization and mitogen-activated protein kinase activation of the human prostaglandin EP4 receptor". FEBS Letters. 501 (2–3): 156–60. doi:10.1016/S0014-5793(01)02640-0. PMID 11470276. S2CID 29938003.
- Slipetz D, Buchanan S, Mackereth C, Brewer N, Pellow V, Hao C, Adam M, Abramovitz M, Metters KM (October 2001). "Sequestration and phosphorylation of the prostaglandin E2 EP4 receptor: dependence on the C-terminal tail". Biochemical Pharmacology. 62 (8): 997–1012. doi:10.1016/S0006-2952(01)00742-0. PMID 11597569. S2CID 25415232.
- Fujino H, West KA, Regan JW (January 2002). "Phosphorylation of glycogen synthase kinase-3 and stimulation of T-cell factor signaling following activation of EP2 and EP4 prostanoid receptors by prostaglandin E2". The Journal of Biological Chemistry. 277 (4): 2614–9. doi:10.1074/jbc.M109440200. PMID 11706038.
- Mutoh M, Watanabe K, Kitamura T, Shoji Y, Takahashi M, Kawamori T, Tani K, Kobayashi M, Maruyama T, Kobayashi K, Ohuchida S, Sugimoto Y, Narumiya S, Sugimura T, Wakabayashi K (January 2002). "Involvement of prostaglandin E receptor subtype EP(4) in colon carcinogenesis". Cancer Research. 62 (1): 28–32. PMID 11782353.
- Kvirkvelia N, Vojnovic I, Warner TD, Athie-Morales V, Free P, Rayment N, Chain BM, Rademacher TW, Lund T, Roitt IM, Delves PJ (February 2002). "Placentally derived prostaglandin E2 acts via the EP4 receptor to inhibit IL-2-dependent proliferation of CTLL-2 T cells". Clinical and Experimental Immunology. 127 (2): 263–9. doi:10.1046/j.1365-2249.2002.01718.x. PMC 1906325. PMID 11876748.
- Asano T, Shoda J, Ueda T, Kawamoto T, Todoroki T, Shimonishi M, Tanabe T, Sugimoto Y, Ichikawa A, Mutoh M, Tanaka N, Miwa M (April 2002). "Expressions of cyclooxygenase-2 and prostaglandin E-receptors in carcinoma of the gallbladder: crucial role of arachidonate metabolism in tumor growth and progression". Clinical Cancer Research. 8 (4): 1157–67. PMID 11948128.
- Kyveris A, Maruscak E, Senchyna M (March 2002). "Optimization of RNA isolation from human ocular tissues and analysis of prostanoid receptor mRNA expression using RT-PCR". Molecular Vision. 8: 51–8. PMID 11951086.
- Scandella E, Men Y, Gillessen S, Förster R, Groettrup M (August 2002). "Prostaglandin E2 is a key factor for CCR7 surface expression and migration of monocyte-derived dendritic cells". Blood. 100 (4): 1354–61. doi:10.1182/blood-2001-11-0017. PMID 12149218.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.