The inferior pharyngeal constrictor muscle is a skeletal muscle of the neck. It is the thickest of the three outer pharyngeal muscles. It arises from the sides of the cricoid cartilage and the thyroid cartilage. It is supplied by the vagus nerve (CN X). It is active during swallowing, and partially during breathing and speech. It may be affected by Zenker's diverticulum.
| Inferior pharyngeal constrictor muscle | |
|---|---|
 Muscles of the pharynx and cheek. (Constrictor pharyngis inferior visible at bottom left.) | |
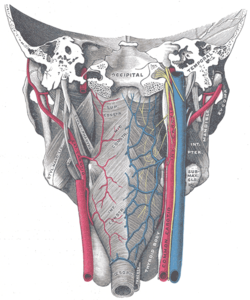 Muscles of the pharynx, viewed from behind, together with the associated vessels and nerves. (Inf. const. labeled at bottom center.) | |
| Details | |
| Origin | Cricoid cartilage and thyroid cartilage |
| Insertion | Pharyngeal raphe |
| Nerve | Pharyngeal plexus of vagus nerve, recurrent laryngeal nerve and superior laryngeal nerve |
| Actions | Swallowing |
| Identifiers | |
| Latin | musculus constrictor pharyngis inferior |
| TA98 | A05.3.01.111 |
| TA2 | 2187 |
| FMA | 46623 |
| Anatomical terms of muscle | |
Structure
editThe inferior pharyngeal constrictor muscle is composed of two parts. The first part (and more superior) arises from the thyroid cartilage (thyropharyngeal part), and the second part arises from the cricoid cartilage (cricopharyngeal part).[1]
- On the thyroid cartilage, it arises from the oblique line on the side of the lamina, from the surface behind this nearly as far as the posterior border and from the inferior horn of the thyroid cartilage.
- From the cricoid cartilage, it arises in the interval between the cricothyroid muscle in front, and the articular facet for the inferior horn of the thyroid cartilage behind.
From these origins, the fibers spread backward and medially to insert with the muscle of the opposite side into the fibrous pharyngeal raphe in the posterior median line of the pharynx. The thyropharyngeal part mainly uses type 2 fibres (anaerobic), while the cricopharyngeal part mainly uses type 1 fibres (aerobic).[2] Fibre type may change after birth.[3]
The inferior fibers are horizontal and continuous with the circular fibers of the esophagus; the rest ascend, increasing in obliquity, and overlap the middle pharyngeal constrictor muscle. The cricopharyngeal part is synonymous with the upper esophageal sphincter (UES), which controls the opening of the cervical esophagus.[4] It is sometimes referred to as the cricopharyngeal inlet.
Nerve supply
editThe inferior pharyngeal constrictor muscle can be supplied by branches from the pharyngeal plexus,[4] the recurrent laryngeal nerve, the external branch of the superior laryngeal nerve, or a combination of these (the recurrent laryngeal nerve being the most common innervation of the cricopharyngeal part).[5] All these branches and nerves come from the vagus nerve (CN X).[4]
Variation
editThe inferior pharyngeal constrictor muscle can merge with superior pharyngeal constrictor, or posterior part of pharyngobasilar fascia.[6]
Function
editThe inferior pharyngeal constrictor muscle has a broad role in moving the lower part of the pharynx.[7]
Swallowing
editAs soon as a bolus of food is received in the pharynx, elevator muscles relax, and the pharynx descends. The inferior pharyngeal constrictor muscle, along with the other constrictors, contract upon the bolus, and convey it downward into the esophagus.[4][7] During swallowing, they contract and cause peristalsis in the pharynx.[4]
Breathing
editThe inferior pharyngeal constrictor muscle is partially used during breathing and speech.[4] It helps to keep the pharynx open, particularly during sleep.[8]
Clinical significance
editZenker's diverticulum
editUncoordinated muscle contraction, cricopharyngeal spasm, or impaired relaxation of the inferior pharyngeal constrictor muscle are currently considered the main factors in development of a Zenker's diverticulum. Zenker's diverticulum develops between the two muscular bellies (the thyropharyngeal part and the cricopharyngeal part) in a small gap called Killian's dehiscence. A diverticulum can form where a balloon of mucosa becomes trapped outside the pharyngeal boundaries. Food or other materials may reside here, which may lead to infection. Motor incoordination of the cricopharyngeal part can cause difficulty swallowing.
In extreme cases, this can be related to retrograde cricopharyngeal dysfunction (R-CPD) which causes the inability to burp; this is in part due to the muscle not being able to relax. Botox or a cricopharyngeal myotomy are used to treat the condition.[9][10]
Radiological damage
editThe inferior pharyngeal constrictor muscle may be damaged by chemotherapy-intensity modulated radiotherapy.[11] This may lead to dysphagia, causing continued use of a feeding tube rather than independent swallowing.[11]
Additional images
edit-
Muscles of the neck. Lateral view.
-
Side view of the larynx, showing muscular attachments.
-
Inferior pharyngeal constrictor muscle
-
Deep dissection of larynx, pharynx and tongue seen from behind
See also
editReferences
editThis article incorporates text in the public domain from page 1142 of the 20th edition of Gray's Anatomy (1918)
- ^ Origin, insertion and nerve supply of the muscle at Loyola University Chicago Stritch School of Medicine
- ^ Hyodo, Masamitsu; Aibara, Ryuichi; Kawakita, Seiji; Yumoto, Eiji (1998-01-01). "Histochemical Study of the Canine Inferior Pharyngeal Constrictor Muscle: Implications for its Function". Acta Oto-Laryngologica. 118 (2): 272–279. doi:10.1080/00016489850155017. ISSN 0001-6489. PMID 9583798.
- ^ Masamitsu Hyodo, Eiji Yumoto, Seiji Kawakita, Takahiko Yamagata (1999-01-01). "Postnatal Changes in the Types of Muscle Fibre in the Canine Inferior Pharyngeal Constrictor". Acta Oto-Laryngologica. 119 (7): 843–846. doi:10.1080/00016489950180522. ISSN 0001-6489. PMID 10687945.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e f Mu, Liancai; Sanders, Ira (2001). "Neuromuscular compartments and fiber-type regionalization in the human inferior pharyngeal constrictor muscle". The Anatomical Record. 264 (4): 367–377. doi:10.1002/ar.10020. ISSN 1097-0185. PMID 11745092. S2CID 22153114.
- ^ Uludag, Mehmet; Aygun, Nurcihan (2016). "Innervation of the human cricopharyngeal muscle by the recurrent laryngeal nerve and external branch of the superior laryngeal nerve". Langenbecks Arch Surg. 402: 683–690. doi:10.1007/s00423-016-1376-5. PMID 26843022.
- ^ Bui, Toai; M Das, Joe (2022), "Anatomy, Head and Neck, Pharyngeal Muscles", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31869118, retrieved 2022-07-22
- ^ a b Yamaoka, Minoru; Furusawa, Kiyofumi (May 1997). "Function of the Inferior Pharyngeal Constrictor Muscle". Dysphagia. 12 (3): 171. doi:10.1007/BF03500907. ISSN 0179-051X. PMID 9190104. S2CID 44633854.
- ^ Sherrey, John H.; Pollard, Marcus J.; Megirian, David (1 April 1986). "Respiratory functions of the inferior pharyngeal constrictor and sternohyoid muscles during sleep". Experimental Neurology. 92 (1): 267–277. doi:10.1016/0014-4886(86)90140-8. ISSN 0014-4886. PMID 3956654. S2CID 7751627.
- ^ Bastian, Robert W.; Hoesli, Rebecca C. (2020). "Partial Cricopharyngeal Myotomy for Treatment of Retrograde Cricopharyngeal Dysfunction". Oto Open. 4 (2): 2473974X2091764. doi:10.1177/2473974X20917644. PMC 7163242. PMID 32328538.
- ^ Bastian, R. W.; Smithson, M. L. (2019). "Inability to Belch and Associated Symptoms Due to Retrograde Cricopharyngeus Dysfunction: Diagnosis and Treatment". Oto Open. 3 (1): 2473974X19834553. doi:10.1177/2473974X19834553. PMC 6572913. PMID 31236539.
- ^ a b Vlacich, Gregory; Spratt, Daniel E.; Diaz, Roberto; Phillips, John G.; Crass, Jostin; Li, Chung-I; Shyr, Yu; Cmelak, Anthony J. (1 March 2014). "Dose to the inferior pharyngeal constrictor predicts prolonged gastrostomy tube dependence with concurrent intensity-modulated radiation therapy and chemotherapy for locally-advanced head and neck cancer". Radiotherapy and Oncology. 110 (3): 435–440. doi:10.1016/j.radonc.2013.12.007. ISSN 0167-8140. PMID 24440043.
External links
edit- lesson8 at The Anatomy Lesson by Wesley Norman (Georgetown University) (latpharyngealitems3)